Category: Health and Well-being
Everything to Know if You Want to Live and Age in Place
June 1, 2025

Most people would prefer the comfort of having their own space as they age. Studies show that as many as 90 percent of adults wish to remain home. Living in place, sometimes known as aging in place, also equates to maintaining independence for as long as possible.
“For many of us, home is comfort. There’s a history we are familiar with: It’s family, friends and neighbors. It reflects our culture and our community,” says Emily Johnson, a licensed clinical social worker. “As we begin to lose control of other aspects of our life, staying in our home says, ‘I can accept help, but I am still running the show.”’
Remaining home as you grow older requires careful consideration and thoughtful planning. Here’s everything you need to know about living and aging in place.
Make Your Plans Now
The best thing to do if you want to age in place is to plan for it now while you are still able to. Consider what kind of help you may need now or want in the future. Planning ahead gives you time to set up your home and budget for the required changes and services.
Be sure to factor in any health conditions you or your spouse may already have. Think about how that condition may make it difficult to care for yourself independently. Then, talk to family and friends about what level of support they can offer. Ensure everyone’s realistic and plan to revisit the issue periodically over time.
On average, an adult over the age of 65 falls every second in the U.S. You can prevent accidents at home with these simple safety measures:
- Apply contrasting colored electrical tape on stair landings.
- Remove throw rugs without grip from the home.
- Clear away clutter, including loose cords.
- This includes the outdoors; porches and walkways should be swept and shoveled.
- Ensure the home is well-lit and place night lights in halls and bathrooms.
- Always use handrails and install grab bars in showers and tubs and next to the toilet.
- Always wear proper-fitting supportive shoes in the house and outdoors.
As conditions change, you may need to reassess your home regularly for potential hazards. To troubleshoot, ask a family member or friend to complete a walkthrough with you for a second set of eyes.
Budget For Services
Home-based care services can be used in short-term situations, such as during recovery from surgery, or in the long term for those who need ongoing help. In addition to healthcare services, people may need help with chores, meal delivery, or transportation for doctor’s visits.
While home-based services can be expensive, they may cost far less than moving into an assisted living facility. The Eldercare Locator is a resource that connects people to caregivers through local support services.
People often rely on various payment sources, including personal funds, long-term care insurance, and government programs. For more information on government-based healthcare and financial assistance, visit USA.gov.
Prioritize Your Long-Term Health
If your goal is to stay home, then make your overall health maintenance a top priority. Stay current with your doctor’s visits and set alarm reminders for medications.
Make a plan to maintain body strength as you age, powerful legs to support balance and assist you in getting up safely from a seated position. “Strength, balance, and flexibility exercises are key to preventing falls, which are among the greatest threats to our healthy longevity,” says Scott Kaiser, a family physician and geriatrician.
In addition to scheduling regular exercise into your routine, don’t forget about your mental well-being. “Investing in meaningful relationships is one of the most important things we can do to increase our health, quality of life, and wellbeing,” says Kaiser. Remain engaged in social activities and plan visits with loved ones, including video calls with those who live farther away.
Prepare for the Unexpected
Always be prepared for unexpected events and medical emergencies. “Be proactive,” says Johnson. “Where are there gaps now or barriers to living independently in the future?” For instance, if you have a preexisting allergy or medical condition like diabetes, wearing a medical alert ID bracelet is a simple precaution. A wearable electronic monitor that can alert emergency personnel in the event of a fall is another easy measure to implement.
Even if the plan is to stay at home for as long as possible, there may come a time when that’s no longer safe. The decision about whether or not to move away from home is a difficult and emotional one to make.
It’s best to mentally prepare for that possibility now while there’s still time to have some control over where you’ll go. Learn as much as possible about the available housing options and include loved ones in the search.
Living in place is an attainable goal with the right amount of forethought. At Insureyouknow.org, you may store all of your financial and medical records in one easy-to-review place. By staying on top of your budget and health needs, you will have already taken care of the most critical components of your aging-in-place plan.
Choosing the Right Care Center for Loved Ones
May 15, 2025

Moving a loved one into a care facility is an important decision that requires careful consideration. Choosing the right one takes in-depth research to determine if it’s a good fit for the individual’s needs. There are nearly 31,000 assisted living centers in the U.S. The first step in finding care is understanding the difference between types of facilities and whether they can provide the level of attention the patient needs.
Types of Care Centers
A nursing home provides around-the-clock medical care for individuals who will likely remain there until their passing. These are meant for individuals who can no longer care for themselves independently or be cared for by their loved ones at home. A skilled nursing facility may be intended for a short or long period. Still, it provides a higher level of medical attention and is usually for those recovering from surgery or an illness.
Independent living and assisted living centers are for those who need less intensive medical assistance but still require some level of care. A continuing-care center can serve as an intermediary between assisted living and a nursing home. For individuals who need 24/7 care and supervision due to Alzheimer’s or dementia, there are memory care centers that specialize in those specific needs.
Paying for Long-Term Care
Many people are unaware that there is no federal assistance available for long-term care costs. There is one exception in which Medicare will pay for the first 100 days in a nursing home or skilled nursing facility if the patient has been hospitalized for at least three consecutive days within the last year before needing to be transferred to a care facility.
Paying for care can be a significant issue for families as it can become costly. “Nursing homes are one of the most expensive levels of care,” says Amie Clark, a senior care expert. “And most people don’t have that kind of money.”
Long-term care insurance policies may be a wise, proactive investment, but they can also be expensive. In most cases, people pay privately or out of pocket until their resources are used up. According to the NCHS, 62% of nursing home residents use Medicaid as their payment source.
Other Factors to Consider
Unfortunately, nursing homes face their fair share of challenges, such as being understaffed or dealing with infectious outbreaks. This is why it’s so important for families to do their due diligence in researching facilities and not feel rushed into making a decision.
Medicare offers an online resource to find and compare nursing homes, hospitals, and other care facilities in your area. It uses a five-star rating system and provides information about each nursing home, including vaccination rates and inspection reports. Another helpful resource is the Nursing Home Inspect, which compiles nursing home inspection reports.
Experts suggest not relying on ratings alone and focusing on a facility’s staffing, saying that nothing beats an in-person visit.
Here’s what to do when you’re on-site:
- Speak with a range of employees, from administrators to activity managers to culinary directors.
- Take note of response times.“How long does it take for call lights to be responded to?” says Shannon Gimbel, manager of the ombudsman program for Denver’s Area Agency on Aging. “Are residents standing in hallways waiting for medication?”
- Notice the patients’ level of hygiene. “Listen in the hallways,” says Tony Chicotel, attorney for the patient advocacy group California Advocates for Nursing Home Reform. “Look at the hair, clothing, teeth, and fingernails of the residents.”
- Try the food. Sit in the dining hall with other residents and observe the interactions between patients and staff.
- Ask about the activities offered to residents and consider whether or not they will be intellectually stimulating.
While it’s best to find a care facility that’s close to you, traveling farther for the best fit may become necessary.
Once you determine what kind of facility your loved one needs and make payment plans, then you should do your research and take the time to visit all of the centers you’ve narrowed down on your list. With Insureyouknow.org, you may compile your research, keep track of finances, and store your loved one’s medical records in one easy-to-review place. While it will take some research, finding the right place will provide you with invaluable peace of mind.
How Much Sleep Do You Really Need?
May 1, 2025

You might pride yourself on burning the midnight oil or think you’re functioning fine on five or six hours of sleep—but your body would likely disagree. According to the CDC, a third of all adults in the United States report that they don’t get enough sleep, and that’s troublesome since the benefits of a good night’s rest are numerous. Sleep isn’t just downtime—it’s when your brain files memories, your body repairs itself, and your mood resets.
So how much sleep do you actually need to feel your best? It’s not a one-size-fits-all answer. While many people are under the assumption they can operate on less than seven hours of sleep a night, research shows that seven hours is just the bare minimum needed.
Here’s everything you need to know about how long you should aim to sleep nightly.
Seven Hours Isn’t Exactly the Golden Rule
According to the CDC, the average adult between the ages of 18 and 60 needs at least seven hours of sleep. “Some people need less than seven hours, while others might need more,” says Eric Zhou, a psychologist at the Division of Sleep Medicine at Harvard Medical School.
While people usually focus on the amount of sleep they need, they forget to consider the quality of sleep they’re having. For instance, you may go to bed at 11 p.m. with an alarm set for 6 a.m., but when do you actually fall asleep, and are you staying asleep all night?
“Instead of focusing exclusively on the number of hours we sleep per night, we should also consider our sleep quality,” says Zhou. It’s about the time you spend in bed every night, but it’s more about the amount of uninterrupted deep sleep you’re experiencing nightly.
Wearable sleep trackers, such as the Oura Ring, Fitbit, or Apple Watch, can provide valuable insight into your patterns and help you develop better sleep habits.
Women May Require More Sleep
The traditional estimate of nightly seven to nine hours of sleep is based on studies that only involved men. This has recently led many to wonder whether or not women need more sleep than men, and several factors suggest they may.
Since women are often caregivers, they are wired to multitask and use more of their brain, while they also report higher levels of stress. This mental exhaustion alone could account for them requiring slightly more sleep every night.
The other factor is hormonal, depending on where they are in their cycle each month, as well as during pregnancy and even after menopause. For instance, the hormone progesterone, which peaks at different times, is a relaxing hormone and often leads to drowsiness.
While not everyone agrees, many health professionals are beginning to recommend more sleep for women, who probably need at least eight hours of sleep a night.
Factoring in Age
The younger you are, the more sleep you need, especially when the body is growing or going through major changes. A newborn needs up to 17 hours of sleep a day, while a teenager between the ages of 13 and 18 needs up to ten.
As you age, melatonin production, which is the sleep hormone, declines. The result of less melatonin is waking up earlier or waking up throughout the night. Once over the age of 61, getting the recommended amount of nine hours of sleep can become more challenging.
How to Get a Good Night’s Sleep
Consistency is key for a good night’s sleep. Try maintaining the same time window between lying in bed and waking up. This works because the body recognizes routine and can be trained to sleep within a specific time frame. “People with good sleep quality often have a predictable sleep window where their sleep occurs,” says Zhou. “Good sleepers are likely to sleep around the same number of hours and stay asleep through the night.”
Physical activity during the day also influences how well you sleep at night. The more activity you incorporate into your day will directly correlate to how much sleep your body needs and therefore, how tired you’ll be by bedtime. “Activity increases your sleep drive,” says Dr. Michelle Drerup, a sleep medicine psychologist. “It’s important to develop exercise as a habit. Pick a time of day that works for you and exercise at the same time every day.”
Refraining from eating two to four hours before bedtime can also help. When we eat, the body must switch gears to digestion, so when you eat right before bed, you must focus on digesting that food and cannot fall into a deep sleep. Eating before bedtime robs your body of its capacity to concentrate on the work it does while you’re sleeping.
The same rule applies to nightly screen time. Studies show that two or more hours of screen time in the evening can disrupt the rise in melatonin you need to fall asleep. Turn devices off at least one hour before bedtime, and replace scrolling with reading a book, taking a bath, or meditating. If you must use your phone at night, reduce your blue light exposure by turning down the brightness or switching to nighttime mode in the evening.
Building a routine that you can stick to ensures the right amount of sleep every night is possible. With Insureyouknow.org, you can store your medical records in one easy-to-review place. The effort you put into a good night’s rest will show in time.
Everything to Know About Equine-assisted Psychotherapy
March 14, 2025

Horses are well known for the special connection they form with their owners, but bonding with horses is not only more accessible than ever, it can be healing. Beyond pet companionship, horses can be used in therapeutic settings to help people process challenging emotional experiences.
During equine-assisted psychotherapy (EAP), people may groom, feed, or lead a horse with a mental health professional nearby. The main goal of this form of therapy is to help patients with emotional regulation. EAP differs from traditional talk therapy as it offers a more inviting setting, brings people outside, and allows them to use all their senses while processing emotions.
How Horse Therapy Differs From Traditional Counseling
Unlike humans, horses bring different qualities to therapy. For example, horses cannot give patients a feeling of bias or judgement, but because they are sensitive to emotions, they still convey a sense of understanding and connection. “They’re sentient beings, and they think and feel and have incredible memories,” says Paige Deponte, director of an equine-assisted trauma-informed care organization in Honokowai, Hawaii. “They were made to do this.”
Plus, horses’ care, such as feeding and grooming, is therapeutic and helps build empathy. The horse’s unique nature gives people a better awareness of their emotions, increased adaptability, stress tolerance, and even self-esteem. “The goal is for the client to find out more about their needs through a series of questions,” says Depontei. “No session is ever the same.”
Horses Have Been Used in Therapy Throughout History
Hippocrates, the Greek physician known as the “Father of Medicine,” wrote about the therapeutic benefits of horseback riding around 400 BCE. Around the world, horses have even been used to heal specific physical ailments. Scandinavia used equine therapy to treat patients with myelitis in 1946, and in 1952, the Olympian Liz Hartzel credited the healing power of horses as helping her recover from polio.
Riding became a popular form of therapy in the 1950s and 1960s. The North American Riding for Handicapped Association was formed in 1969 and eventually became the Professional Association of Therapeutic Horsemanship International, recognized as PATH. By the 1980s, American and Canadian therapists created a more structured Hippotherapy model to be referenced for treatment.
The Benefits of Horse-Assisted Therapies
Equine-assisted forms of therapy are becoming more popular because of increasing evidence of their effectiveness. “I think it’s growing, and the benefits of it are commanding attention because it is unique,” says Whitney Diamond, who breeds and trains horses for a living. “A huge part of the reason why I believe that the therapy is so powerful with horses is that they’re so primal.”
It’s thought that since they’ve been domesticated for some time, horses are attuned to human emotions and nonverbal signals. This allows them to mirror what someone is feeling, enabling the patient to recognize their mental state. “A big part of therapy is that you must work with them,” says Diamond. “It’s powerful because you have this other being that’s not judging you, that’s working off synergy and energy, and they’re going to meet you where you’re at, good or bad.”
EAP is shown to be just as effective in children, teens, and adults and may be used to help with anxiety, depression, and trauma. EAP can benefit young children who find it challenging to open up and process painful experiences.
There are also physical benefits from working with horses. Caring for an animal is shown to decrease blood pressure and improve cholesterol levels. Horses in particular encourage socialization through other riders, which can lessen feelings of loneliness and isolation. Vigorous horseback riding is also a great cardiovascular exercise, while grooming the horse and taking care of equipment can help build strength.
How to Find a Treatment Center Near You
You may reference PATH Intl. or the Equine Assisted Growth and Learning Association to find an EAP certified professional. These are the most reputable organizations that set the standard, train, and certify anyone using horses as a part of therapy.
Those who are interested in trying EAP are advised to find a program that specializes in their specific difficulty, such as anxiety or trauma recovery. The mental professional at the given organization will then be able to tell potential clients whether or not they seem like a fit for the program.
If you have any physical limitations, especially back injuries, then EAP might not be the right fit for you. Other considerations include a fear of horses and the cost of therapy, which may not be covered through insurance.
If you or a loved one may benefit from equine-assisted therapy, you may look for an organization that takes your insurance or offers affordable care. With Insureyouknow.org, you may keep your medical records and progress reports in one easy-to-access place. By keeping track of the changes you notice during therapy, you can observe how you benefit from this unique form of connection in many different ways.
Medicare Grocery Allowances: Who Qualifies and Is it Worth it?
January 15, 2025

In 2020, the Medicare Advantage expanded coverage benefits for those with chronic conditions, such as cancer, autoimmune disorders, diabetes, end-stage renal or liver disease, heart disease, and more. The coverage expansion is referred to as the special supplemental benefits for the chronically ill or SSBCI. Some additional benefits include food allowances and prepared meals, but in some instances, they may even include over-the-counter medications, transportation, and in-home support services.
If you’re interested in receiving a grocery allowance or meal benefits or need food assistance, here’s everything you need to know about the additional coverage.
How the Medicare Grocery Allowance and Meal Benefits Work
Grocery allowances and meal benefits are not the same. If you qualify for grocery allowances, they are issued through prepaid debit cards on a monthly or quarterly basis. While the grocery allowance varies by state, it is usually $50 each quarter.
Under the CHRONIC Care Act, as of 2020, Medicare Advantage plans could also provide meals anytime to keep eligible recipients from needing hospitalization. Meal benefits are often more popular than grocery allowances, but it’s usually only offered for a limited amount of time, which is typically four weeks after a hospital stay.
Knowing Which Plans Offer Food Assistance
Not all Medicare Advantage plans include food allowances, so it’s important to determine if you qualify before choosing a plan. Traditional Medicare Part A and Part B and Medicare supplement plans, which are meant to supplement gaps in coverage, do not offer a grocery allowance. Some Part C Medicare Advantage Plans do offer grocery allowances and meal benefits, such as special needs plans or SNPs and dual-eligible special-needs plans D-SNPs. D-SNPs are meant for Medicare members who are also enrolled in Medicaid and who have a chronic condition. Those with Medicare Advantage plans who are disabled or who have a low-income subsidy or LIS may also be eligible to receive grocery benefits.
The CHRONIC Care Act of 2020 gave Medicare Advantage plans the ability to offer non-medical benefits such as funds for groceries. “Therefore, the Medicare Advantage plan can decide if they want to provide those benefits, and those benefits have to be designed only for the chronically ill,” says Alexandra Ashbrook, director of the Food Research and Action Center. “The non-medical services have to be targeted to people who have at least one chronic health condition, such as those at risk of hospitalization or some other adverse health outcome requiring intensive care coordination,” she says.
Qualifications for the grocery and meal benefits vary by plan, so it’s important to check with the plan’s provider to see what they offer and if your health condition qualifies. Choosing a plan based solely on food allowances isn’t the best approach over the long run. So, even if the plan offers a grocery or meal benefit, it may not justify what you pay for the plan. Whether or not the plan covers medical needs should always be the priority. Take into account every benefit the plan offers before making a decision.
What to do if You Don’t Qualify for Medicare Food Allowances
There are still other options for those who do not qualify for the grocery allowance through their Medicare Advantage Plan. Low-income seniors 60 or older can apply for food assistance through the Supplemental Nutrition Assistance Program or SNAP. Many people don’t even realize that they qualify for these benefits. “Unfortunately, only about 48% of eligible older adults are participating in SNAP,” Ashbrook says. “That’s a really important gap that health care providers and health systems could help to close before looking at any of the other additional food programs.”
Those who are 60 or older and have an income below 185% of the federal poverty income guidelines may also qualify for the Senior Farmers’ Market Nutrition Program SFMNP or the Commodity Supplemental Food Program or CSFP. The SFMNP provides coupons for fresh fruits and vegetables, which can be used at farmers’ markets and community farms, while the CSFP is a monthly package of healthy food that the USDA distributes to local agencies for participants to pick up. If eligible, some states even offer package deliveries.
To find out if you are eligible for SNAP or either of these additional programs, you may fill out an application online. If you’re a veteran, for instance, you may be more likely to qualify for USDA food assistance programs. Even if you are not eligible for Medicare grocery allowances, SNAP, or other supplemental programs, you still have options. Meals On Wheels is another program designed to help low-income seniors access prepared meals. The meals are provided on a sliding scale based on a recipient’s income to make them an affordable option for those in need.
If any food assistance will help you, then exploring every available benefit will pay off. Whether it’s a Medicare food allowance or a USDA-based food assistance program, helping purchase and prepare healthy foods can go a long way in improving the quality of your everyday life. With Insureyouknow.org, you may keep track of your applications, health records, and grocery budgets in one easy-to-access place for all your meal planning needs.
The Health Benefits of Even the Shortest Vacations
December 15, 2024

Just like an athlete benefits from breaks during exercise, vacations are an important part of someone’s well-being. According to a Pew Research Center survey in 2023, nearly half of the U.S. workers surveyed said they take less time off than the paid time off their employers gave them, while globally, eighty-five percent of workers reported that vacations make them feel more optimistic and that regular vacations are important for their overall health.
“Not taking time off from work to go on vacation or simply rest can lead to overwork and burnout,” says Joyce Marter, a licensed psychotherapist. “People should use all the vacation time allotted to them—and sick days should also be used.
If you’ve been feeling the need for a true rest, here’s everything you need to know about getting the most out of even the shortest vacations.
The Right Amount of Time Off
While experts agree that any amount of vacation time is beneficial, three weeks per year may be just the right amount to benefit your health. The European Society of Cardiology conducted a 40-year-long study that found people who take less than three weeks of vacation time per year have a 37% greater risk of premature death, even despite living an otherwise healthy lifestyle.
Another study in 2020 showed that people who split two weeks of annual vacation time into five short breaks had a 24% lower risk of metabolic syndrome. Even the long weekend can come with serious benefits, as those who took a four-day vacation had improved stress-levels for an entire month after returning to work.
Since the positive effects of a trip usually fade after a month of being back home, taking several short trips throughout the year can be more beneficial than one or two long vacations. Plus, the planning process can make you feel happier than the trip itself, so allowing yourself to plan and look forward to a trip more often throughout the year extends the benefits of your vacation time even more.
The Right Way to Travel
Simply going on vacation won’t necessarily result in feeling as though you have a break. “I’ve heard countless times how exhausted people are when they come back from their vacation and feel like they ‘need a vacation from their vacation,’ and that’s because many times we pack so much into a very short amount of time,” says Esther Susag, a travel blogger. “We want to see everything, do everything, and not waste a minute.”
In order to benefit from any amount of time away, it’s important that you provide yourself with the opportunity to actually rest.
Slow travel is a more meditative approach to traveling that allows people to slow down, as the name suggests, and literally stop and smell the roses. “If you want to really unplug and relax without the stresses of traveling then slow travel may be for you,” says Mark Wolters, a YoutTube travel channel host. “You get to unpack your suitcases less, take fewer planes, trains and automobiles and just relax in a destination.
Once you’re on vacation, give yourself the gift of a loose plan. Do some research ahead of time and bring a list of some things you don’t want to miss when you’re there, as well as a few restaurant possibilities. For every day that you’re there, have a half day’s worth of activities planned, giving yourself the time and space in each place to really enjoy the experience.
The Right Companion
In order to have a truly beneficial break, it becomes important to choose the people you vacation with carefully. “Spending time with family and friends are all things that we know can increase well-being and even reduce stress,” says Stephanie Preston, psychology professor at the University of Michigan. “There can be a lot of interpersonal conflict over how you manage the schedule and the priorities.”
While the idea of traveling with extended family, for instance, seems like a good idea on paper, trying to please everyone may prove to be the opposite of a relaxing getaway.
That being said, vacations can also provide the opportunity to bond with your family members and create truly lasting connections with one another. When you plan to travel slowly, your adventure becomes more about being together as a family than about visiting as many attractions as possible. Slow travel provides the space not only to notice your surroundings but also to notice the people you are seeing them with.
The Right Location
Once you decide who to travel with, opt to stay at a vacation rental rather than a hotel. Rentals are rarely at the center of the tourist attractions. This provides both a more relaxing environment to unplug in but also immerses you more deeply into the local experience. Plus, with rentals that have fully stocked kitchens, there’s less of a reason to have to leave and more of an opportunity to stay in and unwind.
The Right Format
Most people intuitively sense that taking a break is good for their health. What’s most important for people to realize is that they don’t need a vacation to have a break. “Many people don’t often have a choice in how much rest is available to them,” says Julia Kocian, a social worker and mental health counselor. “The way society is set up, we treat rest as a privilege, not a right,” she says.
Whether it’s taking a walk in the evening or meditating while you fold the laundry, only you will know what activities best help you to relax. “I view rest as intentionally slowing down or stepping away from an activity, while taking a break can be more active, like going on a walk or stretching,” says Samantha Artherholt, a psychologist and professor at UW School of Medicine. “The goal of any sort of rest or break is it should feel relaxing. You should feel refreshed and better after the break than you did before.”
Work yourself up towards taking more vacation time by finding ways to distribute downtime throughout your day and week. “The biggest thing is giving yourself permission to do it,” Artherholt says. When you learn more about what feels like rest to you, then you can start planning a handful of short vacations for yourself throughout the year. With Insureyouknow.org, you may store your destination research, savings goals, and travel plans all in one place. Remember that planning for your next vacation may be over half of the fun.
Understanding What Hospice Care Means
July 1, 2024

When treatment for serious illnesses is causing more side effects than benefits, or when health problems become compounded, then a patient and their family members may begin to wonder about hospice. “We recognized as people consider hospice, it’s highly emotional times,” says medical director for Austin Palliative Care Dr. Kate Tindall. “It might include worries and fears.” But one of the things she hears most often from patients and their families is that they wish they had started sooner. Understanding who qualifies for hospice and what it entails is the first part of deciding what might be best for those with terminal conditions.
What is Hospice Care?
Hospice is meant to care for people who have an anticipated life expectancy of 6 months or less, when there is no cure for their ailment, and the focus of their care shifts to the management of their symptoms and their quality of life. With hospice, the patient’s comfort and dignity become the priority, so treatment of the condition ends and treatment of the symptoms, such as pain management, begins. There are no age restrictions placed around hospice care, meaning any child, adolescent, or adult who has been diagnosed with a terminal illness qualifies for hospice care.
An individual does not need to be bedridden or already in their final days of life in order to receive hospice care. Other common misconceptions about hospice care are that it is designed to cure any illness or prolong life. It is also not meant to hasten death or replace any existing care, such as those already provided by a physician.
Determining When it’s Time for Hospice
Establishing care is most beneficial for the patient and their caregivers when it is taken advantage of earlier rather than later. Hospice can be used for months as long as eligibility has been met. Once there is a significant decline in physical or cognitive function, the goal for treatment should become to help that individual live comfortably and forgo anymore physically debilitating treatments that have been unsuccessful in curing or halting the illness.
Both individuals and their loved ones who would benefit from initiating hospice care are often unaware of the services or are uncomfortable asking about them. “It’s a hard conversation to have,” says professor of medicine and palliative care at the Duke University School of Medicine David Casarett. “Many people really want to continue aggressive treatment up until the very end.” While many wait for their providers to suggest it, it should be understood that if eligibility for hospice has been met, an individual and their caregivers can initiate hospice care on their own.
Establishing Hospice Care
In order to qualify for hospice care, a physician must certify that the patient is medically eligible, which means that the individual’s life expectancy is 6 months or less. Typically, the referral to hospice starts with the attending physician’s knowledge of that person’s medical history, while eligibility is then confirmed by the hospice physician. A hospice care team consists of professionals who are trained to treat physical, psychological, and the spiritual needs of the individual, while also providing support to family members and caregivers. Care is person-centered, with the importance being placed on the coordination of care, setting clear treatment goals, and communicating with all involved parties.
Receiving Care at Home
Hospice care is generally provided in the person’s home, whether it’s a personal residence or a care facility, such as a nursing home. “When people are close to the end of their lives, going to the hospital does not make them feel better anymore,” explains professor of medicine at the University of California Dr. Carly Zapata. “Because there’s not necessarily something that we can do to address their underlying illness.” Staying at home allows the individual to be around their personal things and close to their loved ones and pets, which can provide them with comfort during the end of their life.
What Does Hospice Care Include?
Hospice includes periodic visits to the patient and their family or caregivers but is available 24-7 if needed. Medication for symptom relief is administered, any medical equipment needed is provided, and toileting and other supplies such as diapers, wipes, wheelchairs, hospital beds are provided. What may surprise some people is that hospice patients may even receive physical and occupational therapy, speech-language pathology services, and dietary counseling.
If needed, short-term inpatient care may be established for those who cannot achieve adequate pain and symptom relief in their home setting. Short-term respite care may also become available to help family caregivers who are experiencing or are at risk for caregiver burnout. Bereavement care, or grief and loss counseling, is also offered to loved ones who may experience anticipatory grief. Grief counseling is available to family members for up to 13 months after the person’s death.
Paying for Hospice
The first step in finding a hospice agency is to search for ones that serve your county. If there are several options available, then it’s recommended to talk to more than one and see which agency will best fit the patient’s needs. Adequate research should be conducted since not all hospice agencies provide physical and occupational therapy.
Hospice is a medicare benefit that all Medicare enrollees qualify for, but it may also be covered through private insurance and by Medicaid in almost every state. Military families may receive hospice through Tricare, while veterans with the Veterans Health Administration Standard Medical Benefits Package are also eligible for hospice. Hospice agencies will also accept individual self-pay, while there are also non-profit organizations that provide hospice services free of charge.
Discontinuing Hospice Care
Though it is uncommon, if a patient does improve or their condition stabilizes, they may no longer meet medical eligibility for hospice. If this happens, the patient is discharged from the program. Another situation that sometimes arises is when a person elects to try a curative therapy, such as a clinical study for a new medication or procedure. In order to do that, the patient must withdraw from hospice through what is called revocation. Both children and veterans are exempt from being disqualified from hospice care if they choose to also pursue curative treatments. Any person may always re-enroll in hospice care at any time as long as they meet the medical eligibility.
Opting for Palliative Care
Individuals with chronic conditions or life-threatening illnesses may opt for palliative care, which doesn’t require people to stop their treatments. Palliative care is a combination of treatment and comfort care and can be an important bridge to hospice care if patients become eligible. Because transitioning to hospice care can be an emotional choice, palliative care providers often help patients prepare for that. Many people avoid palliative care because they think it is equal to giving up and that death is imminent, but studies show that for many, palliative care allows them to live longer, happier lives. This is due to the benefits of symptom management and spiritual support.
While hospice care can be difficult to accept, it can provide people with the best quality of life possible in their final days, as well as provide their loved ones with valued support. With Insureyouknow.org, you may keep track of all medical and financial records in one easy-to-review place so that you may focus on caring for your loved one, your family, and yourself during this period of their care.
Five Things Happy Retirees Have in Common
June 15, 2024

The transition into retirement can be difficult, when work no longer provides a sense of identity and accomplishment. The change can be startling, especially when most people don’t switch to part-time schedules on the way out of their full-time careers. “We don’t really shift our focus to, how do we live well in this extra time,” says M.T. Connolly, author of The Measure of Our Age. “A lot of people get happier as they age because they start to focus more on the meaningful parts of existence and emotional meaning and positive experience as finitude gets more real.”
While most people account for how much money they’ll need when it’s time to retire, there are many other factors to consider when planning for a fulfilling retirement. Here are five things that happy retirees have in common.
Feeling a Sense of Purpose
There are several approaches to staying active and finding purpose after leaving a career. “Your retirement schedule should be less stressful and demanding than your previous one, but we don’t need to avoid all forms of work or service,” says Kevin Coleman, a family therapist. “Find some work that you take pride in and find intrinsically meaningful.”
Many retirees, for example, choose encore careers, where instead of working for the money, they are working for the enjoyment of the job. Besides finding a new job, there are other simple ways to feel purposeful during retirement. Purpose can be found by making oneself useful, such as by volunteering in the community, joining a community board, or participating in an enjoyable activity with a group, like a gardening club. Many retirees enjoy volunteering to take care of their grandchildren or helping their older friends with caregiving duties. Finding purpose doesn’t need to be complicated and can be achieved through simple acts of showing up for others and being open to new connections.
Finding Ways to Connect
As nearly 25% of those who are 65 and older feel socially isolated, finding ways to connect are important for mental and physical well-being during retirement. One way to connect is through storytelling. Sharing our stories with the people we care about strengthens our social bonds and helps us feel less lonely. Storytelling also helps people pass down their family memories, especially when we share stories with younger relatives, such as with grandchildren. It’s a nice feeling to think that your memories will live on through your loved ones. “The models we have for aging are largely either isolation or age segregation,” says Connolly. “There’s a loss when we don’t have intergenerational contact. It impoverishes our social environment.” Perhaps the best thing to do as you age is to cherish and foster these relationships with younger relatives.
Making Plans for the Retirement Years
Budgeting for your retirement is crucial to happiness during the retirement years. Successful retirement planning includes paying off debts prior to retiring and saving for unexpected expenses or emergency funds in addition to a standard monthly budget. According to a survey conducted by Wes Moss, author of You Can Retire Sooner Than You Think, the happiest retirees are those who have between $700,000 and $1.25 million in liquid retirement savings, such as stocks, bonds, mutual funds, and cash. His research also found that retirees within five years or less of paying off their mortgages are four times more likely to be happy in retirement. This is because the mortgage payment is typically the most significant expense, so those retirees who own their homes feel safer and more at peace once they no longer have that bill. Plus, not having a mortgage payment due every month dramatically lowers their monthly expenses and can help retirement savings last longer.
Many retirees overlook retirement planning beyond their finances. New research from the Stanford Center on Longevity shows that where someone lives in retirement can affect their longevity. Researchers found that people over the age of 60 who lived in upper-income areas lived longer due to having more access to health and social services. They also credited strong social networks and a sense of community to living longer. So perhaps there’s a city or area that you’ve always dreamed of living in or you’d like to live closer to family. Think about where you want to live when you’re done working and then plan for it before you retire.
Beyond saving up and thinking about where you want to spend your retirement years, setting goals for once you’re in retirement is equally as important. “Research suggests that those who think about and plan for what they will do in retirement in advance are far happier and fulfilled once they actually retire and begin living this phase of life,” says financial planner Chris Urban. “Sometimes it is helpful for people to write down what they plan to do every day of the week, what goals they have, who they want to spend time with and what they want to do with them.”
While your goals before retirement were likely centered around career and finances, it will be important to set different kinds of goals once you’re retired. Having goals doesn’t become less important just because you’re no longer working. “If you really want something, maybe a new romance, then take a concrete step in that direction,” says psychiatry professor Ahron Friedberg. “Don’t ever tell yourself that it’s too late.”
Prioritizing Both Physical and Mental Health
With a full-time career no longer on the schedule, cooking healthy meals at home, getting enough sleep, and finding ways to be more physically active everyday will be easier. It will also be important to keep up on medical appointments and preventive therapies. A study conducted by Harvard shows that even people who become more physically active and adopt better diets later in their lives still lower their risks of cardiovascular illnesses and mortality more than their peers who do not. “Not all core pursuits include physical activity or exercise, but many of the top ones do. I refer to them as the ‘ings’—walking, running, biking, hiking, jogging, swimming, dancing, etc.,” says Moss. “These all involve some sort of motion and exercise.” The most sustainable form of physical activity will be doing more of those activities that you enjoy and that move your body.
In addition to caring for your physical health, focusing on your mental health is just as important, especially as you age. According to Harvard’s Medical newsletter, challenging your brain with mental exercise activates processes that help maintain individual brain cells and stimulate communication between them. So choose something new or that you’ve always wanted to learn. Take a course at a community college or learn how to play an instrument or speak a language. If you enjoy reading, visit the library every week for a new book. If you enjoy helping others learn, then looking into a part-time tutoring job or volunteering to tutor is a way to challenge yourself mentally, connect socially, and feel a sense of purpose.
Prioritizing your overall health includes asking for help when you need it. If you reach a point where you need assistance with daily tasks and activities, then you shouldn’t hesitate to ask for help early. Whether it’s family members or caregiving services, finding help with the things that are becoming difficult for you is the best way to maintain your independence for as long as you can so that you may continue to thrive during your retirement years.
It’s important to think about how you want to spend your retirement before it’s here. While many people only consider their finances when they begin to plan for the future, there are other factors, including how you’ll spend your time, where you’ll live, and your overall health that will impact the quality of your retirement years. With Insureyouknow.org, storing all of your financial information, medical records, and planning documents in one easy-to-review place will help you plan for what can be the best years of your life.
Life After a Stroke: What You Should Know
May 21, 2024
A stroke affects the brain’s arteries and occurs when a blood vessel that brings blood to the brain gets blocked or ruptures. The area of the brain that is supplied with blood by the blocked or ruptured blood vessel doesn’t get the oxygen and nutrients it needs, and without oxygen, nerve cells are unable to function. Since the brain controls one’s ability to move, feel, and think, a stroke can cause injury to the brain that could affect any or all of these functions.
Everyone should know the signs of a stroke and seek immediate medical attention if you think you or someone around you is having a stroke. If you or someone you love has recently had a stroke, then it’s important to understand what happens next.
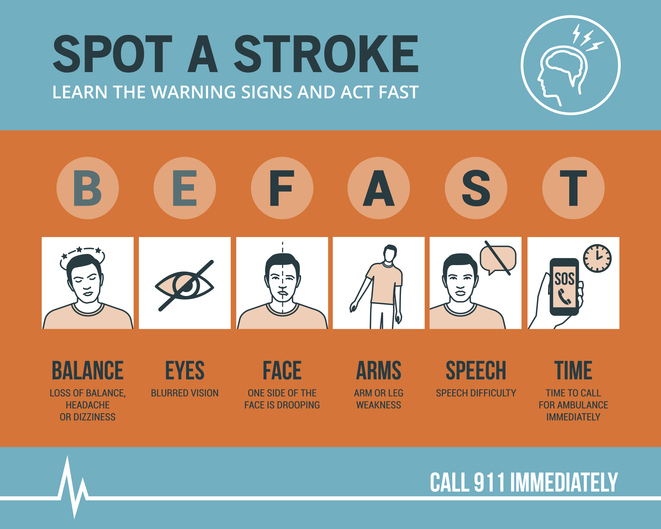
Know the Symptoms of a Stroke and act FAST
The longer the brain is left untreated during a stroke, the more likely it is that someone will have irreversible brain damage. The acronym FAST can help everyone recognize the four main signs that someone may be having a stroke and remember to act fast in seeking medical treatment. That means calling 9-1-1 immediately, as emergency response workers can treat someone on arrival if they think that person is having a stroke.
FAST stands for Facial drooping, Arm weakness, Speech difficulties, and most importantly, Time. If one side of a person’s face is drooping, if the person cannot lift both arms or one arm is drifting downward, and if the person’s speech is slurred or they cannot repeat a simple sentence, then they may be having a stroke. Not all of these signs need to be present to signal a stroke. Just one or two of these symptoms is enough to call 9-1-1, because time is of the essence in the event of a stroke.
Stroke Treatment Begins With Emergency Response Workers
Calling for an ambulance means that the emergency response workers can start life-saving treatment on the way to the hospital. Stroke patients who are taken to the hospital in an ambulance may get diagnosed and treated more quickly than people who wait to drive themselves. The emergency workers may also know best where to take someone, such as to a specialized stroke center to ensure that they receive the quickest possible treatment. The emergency workers can also collect valuable information for the hospital medical staff before the patient even gets to the emergency room, alerting staff of your arrival and allowing time to prepare. All of what the ambulance team can provide saves time in the treatment of stroke, and in the event of a stroke, time is of the essence.
Ischemic Stroke or Hemorrhagic Stroke?
There are two different kinds of stroke, ischemic or hemorrhagic. A medical team will need to determine which kind of stroke the patient is having in order to direct treatment. An ischemic stroke accounts for 87% of all strokes and happens when a blood clot blocks a vessel supplying blood to the brain. Hemorrhagic stroke happens when a blood vessel ruptures and bleeds within or around the brain.
“Fifty percent of strokes present with a clot in a large vessel in the brain, and these don’t respond very well to the old treatment, the IV clot busting medicine,” says M.D. and director of the Sparrow Comprehensive Stroke Center Anmar Razak. “And so nowadays, we do surgery, and what we do is we rush them into the hospital, into the cath lab. We quickly get access through the blood vessels and get up to where the clot is and pull it out.”
With ischemic stroke, the treatment goal is to dissolve or remove the clot. A medication called alteplase or tPA is often administered and works to dissolve the clot and enable blood flow. Alteplase saves lives and reduces the long-term effects of a stroke but must be given to the patient within three hours of the start of a stroke. Then, a procedure called mechanical thrombectomy removes the clot and must happen within six to 24 hours of stroke symptom onset.
For hemorrhagic stroke, the treatment goal is to stop the bleeding. There is a less-invasive endovascular procedure involving a catheter being threaded through a major artery in an arm or leg toward the area of the bleeding in the brain where a mechanism is inserted to prevent further rupture. In some cases, surgery is required to secure the blood vessel that has ruptured at the base of the bleeding.
Rehabilitation After a Stroke
Perhaps the most important part of stroke treatment is determining why it happened or the underlying causes of the stroke. Stroke risk factors include high blood pressure, which weakens arteries over time, smoking, diabetes, high cholesterol, physical inactivity, being overweight, heart disease including atrial fibrillation or aFib, excessive alcohol intake or illegal drug use, and sleep apnea. By making the right lifestyle choices and having a good medical management plan moving forward, the risk of another stroke can be greatly reduced.
That’s because if you have had a stroke, you are at high risk for having another one. One in four stroke survivors have another within five years, while the risk of stroke within 90 days of transient ischemic attack or TIA is as high as 17% with the greatest risk during the first week. This is why it becomes so important to determine the underlying causes of the initial stroke. Your doctor may give you medications to manage a condition, such as high blood pressure, and then recommend lifestyle changes, including a different diet and regular exercise.
Rehabilitation after a stroke begins in the hospital, often within only a day or 2 after the stroke. “There are so many things that patients need to fall into place to be functional and independent again after a stroke,” said Razak. “And they always come down to speed and time.” Rehabilitation can help with the transition from the hospital to home and can help prevent another stroke. Recovery time after a stroke is different for everyone and can take weeks, months, or even years. Some people may recover fully, while others may have long-term or lifelong disabilities. Stroke rehabilitation should be thought of as a balance between full recovery and learning how to live most effectively with some deficits that may not be recovered.
Difficulties from a stroke range from paralysis or weakness on one or both sides of the body, fatigue, trouble with cognitive functioning such as thinking and memory, seizures, and mental health issues like depression or anxiety from the fear of having another stroke. Everyone’s rehabilitation will look different based on their difficulties after a stroke but may include speech, physical, and occupational therapy. Speech therapy helps when someone is having problems producing or understanding speech, physical therapy uses exercises that help someone relearn movement and coordination skills, and occupational therapy focuses on improving daily activities, such as eating, dressing, and bathing. Joining a patient support group may help people adjust to life after a stroke, while support from family and friends can also help relieve the depression and anxiety following a stroke. It’s important for stroke patients to let their medical team and loved ones know how they’re feeling throughout their recovery and what they may need help with.
Stroke rehabilitation can be hard work, but just as in the initial treatment of a stroke, time matters in the possibility of a full recovery. Many survivors will tell you that rehabilitation is worth it and recommend using motivators to achieve recovery goals, such as wanting to see a child’s graduation or returning to working in the garden. With Insureyouknow.org, caretakers may keep track of medical treatments and rehabilitation plans in one easy-to-review place so that they may focus on caring for their loved one during the period of recovery from stroke.
May is American Stroke Month which aims to raise awareness of the second leading cause of death.
Gardening for Mental Well-Being
May 15, 2024

Interest in gardening has increased since the pandemic, as more and more people are searching for ways to disconnect from stressful times and reconnect to nature. It turns out that immersing ourselves in green spaces and caring for plants is a form of caring for ourselves. Time spent in nature has been found to improve mental health so much so that gardening has been prescribed by the National Health Service in Great Britain since 2019. But while scientists are just beginning to pay attention to nature’s overall effect on our health, humans have known about the power of gardening for a very long time.
Historic Gardens and Horticultural Therapy
Ancient and modern gardens all over the world, including Persian pleasure gardens, Islamic paradise gardens, Chinese courtyard gardens and Japanese rock gardens, nurture a sense of separation from the chaotic world and provide a place for inward reflection. In addition to sources of food, the Roman Empire treated gardens as a place to cultivate mindfulness. As extensions of the home, Roman gardens were the first outdoor rooms. They served as spaces to rest and marvel at nature’s wonder. By the Middle Ages, hospital gardens modeled after these Roman gardens were seen as integral parts of the hospital, not just to feed patients and grow medicines but to offer patients time outside. But as efficiency and technology took over medical treatment, these spaces went extinct.
Still, the benefits of gardens were not forgotten. In the 1800s, early American psychiatrists began noting links between horticulture and mental health. Born in 1933, the famous neurologist Dr. Oliver Sacks believed that gardens and nature were more powerful than any medication. As the scientific evidence of spending time in green spaces leading to better health grew, many hospitals began incorporating gardens into their facilities again and horticultural therapy was developed as a therapeutic practice in the 1970s.
Horticultural therapy involves taking care of plants with specific goals for the patient in mind. For instance, tending to a garden and watching it thrive can help people build self-esteem and feel a sense of accomplishment. Gardening can also lead to life lessons, such as when a plant dies, the person can ask themselves, “What could I have done differently?” Connecting the garden to themself can lead them to think that maybe they can do a little more to take care of themself, too. “It’s really the plants that are the therapists,” says Laura Rumpf, a horticultural therapist who treats patients with dementia through gardening. “Even if somebody can’t necessarily name what it is they’re smelling, the body somehow remembers.” For those with dementia for instance, plants can help them to reminisce which leads to telling stories and sharing memories, an important part of connecting to others and validating their identity.
The Scientific Proof of Nature’s Benefits
Gardening involves exercise, which we know is beneficial to our health, and since people tend to breathe more deeply when they’re outside, outdoor activities can clear the lungs, aid digestion, and improve immune responses. Sunlight also lowers blood pressure and increases vitamin D levels, but the benefits of outdoor gardening extend beyond these physical benefits.
A recent study conducted by scientists at the University of Florida found that gardening lowered stress, anxiety and depression in healthy women who attended a gardening class twice a week. “Past studies have shown that gardening can help improve the mental health of people who have existing medical conditions or challenges,” said the principal investigator of the study Charles Guy. “Our study shows that healthy people can also experience a boost in mental well-being through gardening.” In addition to improved mental well-being, interacting with nature has proven cognitive benefits. A 2019 study by University of Chicago psychologist Marc Berman showed that green spaces near schools promote cognitive development in children, while adults assigned to public housing in green neighborhoods exhibited better attentional functioning than those assigned to units with less access to green spaces.
Scientists have a few ideas as to why nature is so good for our mental health. One hypothesis is that since our ancestors evolved in the wild and relied on their environment for survival, we have an innate drive to connect with nature. As a species, we may be attracted to plants because we depend on them for food and shelter. Another hypothesis is that spending time in nature triggers a physiological response that lowers stress levels. Throughout human history, trees and water have been an oasis and signaled relaxation. There is an implicit trust in nature that calms our parasympathetic nervous system. Yet a third hypothesis is that nature replenishes cognitive functioning, which restores the ability to concentrate and pay attention. The truth probably lies in a combination of all of these theories.
Gardening Against Loneliness
Perhaps one of the most overlooked yet obvious benefits of gardening is that it can make people feel less alone in the world. While gardening can bring people together through community gardens, one doesn’t even need to be around other people while spending time in nature in order to feel more connected to others. “Nature can be a way to induce awe,” said psychology professor John Zelenski. “One of the things that may come from awe is the feeling that the individual is part of a much bigger whole.”
Gardening can bring people together through a sense of community, as people who garden are rich with expertise that they are willing to share with other gardeners. Master gardeners and local volunteers dedicate their time to empowering other people in the community who are interested in growing their own plants. Simply sharing a gardening blunder is just one way to connect with a fellow gardener. Social connections are important for our mental well-being because they help lower stress, improve resilience, and provide support, while a strong sense of belonging has been shown to lower one’s risk of depression and anxiety.
Community gardens are a great place to connect with others as they offer room for talking during uncomplicated and repetitive tasks. Since gardening can bring together all kinds of people, time in the garden with others can also remind us that we are more alike than not. “Gardens are a great point of connection,” said the director of a London community garden Sarah Alun-Jones. “We often find ourselves talking about where we grew up, our childhood gardens, food we like to grow and cook… and we learn lots along the way.”
If you’re thinking of incorporating gardening into your routine, it doesn’t need to be intimidating. Simply starting by potting indoor plants or taking walks in green spaces during your lunch break are just two simple ways to connect with nature now. At Insureyouknow.org, you may store all of your gardening plans and records, so that you can become the researcher of your own gardening benefits.
