Category: Health and Well-being
Understanding What Hospice Care Means
July 1, 2024

When treatment for serious illnesses is causing more side effects than benefits, or when health problems become compounded, then a patient and their family members may begin to wonder about hospice. “We recognized as people consider hospice, it’s highly emotional times,” says medical director for Austin Palliative Care Dr. Kate Tindall. “It might include worries and fears.” But one of the things she hears most often from patients and their families is that they wish they had started sooner. Understanding who qualifies for hospice and what it entails is the first part of deciding what might be best for those with terminal conditions.
What is Hospice Care?
Hospice is meant to care for people who have an anticipated life expectancy of 6 months or less, when there is no cure for their ailment, and the focus of their care shifts to the management of their symptoms and their quality of life. With hospice, the patient’s comfort and dignity become the priority, so treatment of the condition ends and treatment of the symptoms, such as pain management, begins. There are no age restrictions placed around hospice care, meaning any child, adolescent, or adult who has been diagnosed with a terminal illness qualifies for hospice care.
An individual does not need to be bedridden or already in their final days of life in order to receive hospice care. Other common misconceptions about hospice care are that it is designed to cure any illness or prolong life. It is also not meant to hasten death or replace any existing care, such as those already provided by a physician.
Determining When it’s Time for Hospice
Establishing care is most beneficial for the patient and their caregivers when it is taken advantage of earlier rather than later. Hospice can be used for months as long as eligibility has been met. Once there is a significant decline in physical or cognitive function, the goal for treatment should become to help that individual live comfortably and forgo anymore physically debilitating treatments that have been unsuccessful in curing or halting the illness.
Both individuals and their loved ones who would benefit from initiating hospice care are often unaware of the services or are uncomfortable asking about them. “It’s a hard conversation to have,” says professor of medicine and palliative care at the Duke University School of Medicine David Casarett. “Many people really want to continue aggressive treatment up until the very end.” While many wait for their providers to suggest it, it should be understood that if eligibility for hospice has been met, an individual and their caregivers can initiate hospice care on their own.
Establishing Hospice Care
In order to qualify for hospice care, a physician must certify that the patient is medically eligible, which means that the individual’s life expectancy is 6 months or less. Typically, the referral to hospice starts with the attending physician’s knowledge of that person’s medical history, while eligibility is then confirmed by the hospice physician. A hospice care team consists of professionals who are trained to treat physical, psychological, and the spiritual needs of the individual, while also providing support to family members and caregivers. Care is person-centered, with the importance being placed on the coordination of care, setting clear treatment goals, and communicating with all involved parties.
Receiving Care at Home
Hospice care is generally provided in the person’s home, whether it’s a personal residence or a care facility, such as a nursing home. “When people are close to the end of their lives, going to the hospital does not make them feel better anymore,” explains professor of medicine at the University of California Dr. Carly Zapata. “Because there’s not necessarily something that we can do to address their underlying illness.” Staying at home allows the individual to be around their personal things and close to their loved ones and pets, which can provide them with comfort during the end of their life.
What Does Hospice Care Include?
Hospice includes periodic visits to the patient and their family or caregivers but is available 24-7 if needed. Medication for symptom relief is administered, any medical equipment needed is provided, and toileting and other supplies such as diapers, wipes, wheelchairs, hospital beds are provided. What may surprise some people is that hospice patients may even receive physical and occupational therapy, speech-language pathology services, and dietary counseling.
If needed, short-term inpatient care may be established for those who cannot achieve adequate pain and symptom relief in their home setting. Short-term respite care may also become available to help family caregivers who are experiencing or are at risk for caregiver burnout. Bereavement care, or grief and loss counseling, is also offered to loved ones who may experience anticipatory grief. Grief counseling is available to family members for up to 13 months after the person’s death.
Paying for Hospice
The first step in finding a hospice agency is to search for ones that serve your county. If there are several options available, then it’s recommended to talk to more than one and see which agency will best fit the patient’s needs. Adequate research should be conducted since not all hospice agencies provide physical and occupational therapy.
Hospice is a medicare benefit that all Medicare enrollees qualify for, but it may also be covered through private insurance and by Medicaid in almost every state. Military families may receive hospice through Tricare, while veterans with the Veterans Health Administration Standard Medical Benefits Package are also eligible for hospice. Hospice agencies will also accept individual self-pay, while there are also non-profit organizations that provide hospice services free of charge.
Discontinuing Hospice Care
Though it is uncommon, if a patient does improve or their condition stabilizes, they may no longer meet medical eligibility for hospice. If this happens, the patient is discharged from the program. Another situation that sometimes arises is when a person elects to try a curative therapy, such as a clinical study for a new medication or procedure. In order to do that, the patient must withdraw from hospice through what is called revocation. Both children and veterans are exempt from being disqualified from hospice care if they choose to also pursue curative treatments. Any person may always re-enroll in hospice care at any time as long as they meet the medical eligibility.
Opting for Palliative Care
Individuals with chronic conditions or life-threatening illnesses may opt for palliative care, which doesn’t require people to stop their treatments. Palliative care is a combination of treatment and comfort care and can be an important bridge to hospice care if patients become eligible. Because transitioning to hospice care can be an emotional choice, palliative care providers often help patients prepare for that. Many people avoid palliative care because they think it is equal to giving up and that death is imminent, but studies show that for many, palliative care allows them to live longer, happier lives. This is due to the benefits of symptom management and spiritual support.
While hospice care can be difficult to accept, it can provide people with the best quality of life possible in their final days, as well as provide their loved ones with valued support. With Insureyouknow.org, you may keep track of all medical and financial records in one easy-to-review place so that you may focus on caring for your loved one, your family, and yourself during this period of their care.
Five Things Happy Retirees Have in Common
June 15, 2024

The transition into retirement can be difficult, when work no longer provides a sense of identity and accomplishment. The change can be startling, especially when most people don’t switch to part-time schedules on the way out of their full-time careers. “We don’t really shift our focus to, how do we live well in this extra time,” says M.T. Connolly, author of The Measure of Our Age. “A lot of people get happier as they age because they start to focus more on the meaningful parts of existence and emotional meaning and positive experience as finitude gets more real.”
While most people account for how much money they’ll need when it’s time to retire, there are many other factors to consider when planning for a fulfilling retirement. Here are five things that happy retirees have in common.
Feeling a Sense of Purpose
There are several approaches to staying active and finding purpose after leaving a career. “Your retirement schedule should be less stressful and demanding than your previous one, but we don’t need to avoid all forms of work or service,” says Kevin Coleman, a family therapist. “Find some work that you take pride in and find intrinsically meaningful.”
Many retirees, for example, choose encore careers, where instead of working for the money, they are working for the enjoyment of the job. Besides finding a new job, there are other simple ways to feel purposeful during retirement. Purpose can be found by making oneself useful, such as by volunteering in the community, joining a community board, or participating in an enjoyable activity with a group, like a gardening club. Many retirees enjoy volunteering to take care of their grandchildren or helping their older friends with caregiving duties. Finding purpose doesn’t need to be complicated and can be achieved through simple acts of showing up for others and being open to new connections.
Finding Ways to Connect
As nearly 25% of those who are 65 and older feel socially isolated, finding ways to connect are important for mental and physical well-being during retirement. One way to connect is through storytelling. Sharing our stories with the people we care about strengthens our social bonds and helps us feel less lonely. Storytelling also helps people pass down their family memories, especially when we share stories with younger relatives, such as with grandchildren. It’s a nice feeling to think that your memories will live on through your loved ones. “The models we have for aging are largely either isolation or age segregation,” says Connolly. “There’s a loss when we don’t have intergenerational contact. It impoverishes our social environment.” Perhaps the best thing to do as you age is to cherish and foster these relationships with younger relatives.
Making Plans for the Retirement Years
Budgeting for your retirement is crucial to happiness during the retirement years. Successful retirement planning includes paying off debts prior to retiring and saving for unexpected expenses or emergency funds in addition to a standard monthly budget. According to a survey conducted by Wes Moss, author of You Can Retire Sooner Than You Think, the happiest retirees are those who have between $700,000 and $1.25 million in liquid retirement savings, such as stocks, bonds, mutual funds, and cash. His research also found that retirees within five years or less of paying off their mortgages are four times more likely to be happy in retirement. This is because the mortgage payment is typically the most significant expense, so those retirees who own their homes feel safer and more at peace once they no longer have that bill. Plus, not having a mortgage payment due every month dramatically lowers their monthly expenses and can help retirement savings last longer.
Many retirees overlook retirement planning beyond their finances. New research from the Stanford Center on Longevity shows that where someone lives in retirement can affect their longevity. Researchers found that people over the age of 60 who lived in upper-income areas lived longer due to having more access to health and social services. They also credited strong social networks and a sense of community to living longer. So perhaps there’s a city or area that you’ve always dreamed of living in or you’d like to live closer to family. Think about where you want to live when you’re done working and then plan for it before you retire.
Beyond saving up and thinking about where you want to spend your retirement years, setting goals for once you’re in retirement is equally as important. “Research suggests that those who think about and plan for what they will do in retirement in advance are far happier and fulfilled once they actually retire and begin living this phase of life,” says financial planner Chris Urban. “Sometimes it is helpful for people to write down what they plan to do every day of the week, what goals they have, who they want to spend time with and what they want to do with them.”
While your goals before retirement were likely centered around career and finances, it will be important to set different kinds of goals once you’re retired. Having goals doesn’t become less important just because you’re no longer working. “If you really want something, maybe a new romance, then take a concrete step in that direction,” says psychiatry professor Ahron Friedberg. “Don’t ever tell yourself that it’s too late.”
Prioritizing Both Physical and Mental Health
With a full-time career no longer on the schedule, cooking healthy meals at home, getting enough sleep, and finding ways to be more physically active everyday will be easier. It will also be important to keep up on medical appointments and preventive therapies. A study conducted by Harvard shows that even people who become more physically active and adopt better diets later in their lives still lower their risks of cardiovascular illnesses and mortality more than their peers who do not. “Not all core pursuits include physical activity or exercise, but many of the top ones do. I refer to them as the ‘ings’—walking, running, biking, hiking, jogging, swimming, dancing, etc.,” says Moss. “These all involve some sort of motion and exercise.” The most sustainable form of physical activity will be doing more of those activities that you enjoy and that move your body.
In addition to caring for your physical health, focusing on your mental health is just as important, especially as you age. According to Harvard’s Medical newsletter, challenging your brain with mental exercise activates processes that help maintain individual brain cells and stimulate communication between them. So choose something new or that you’ve always wanted to learn. Take a course at a community college or learn how to play an instrument or speak a language. If you enjoy reading, visit the library every week for a new book. If you enjoy helping others learn, then looking into a part-time tutoring job or volunteering to tutor is a way to challenge yourself mentally, connect socially, and feel a sense of purpose.
Prioritizing your overall health includes asking for help when you need it. If you reach a point where you need assistance with daily tasks and activities, then you shouldn’t hesitate to ask for help early. Whether it’s family members or caregiving services, finding help with the things that are becoming difficult for you is the best way to maintain your independence for as long as you can so that you may continue to thrive during your retirement years.
It’s important to think about how you want to spend your retirement before it’s here. While many people only consider their finances when they begin to plan for the future, there are other factors, including how you’ll spend your time, where you’ll live, and your overall health that will impact the quality of your retirement years. With Insureyouknow.org, storing all of your financial information, medical records, and planning documents in one easy-to-review place will help you plan for what can be the best years of your life.
Life After a Stroke: What You Should Know
May 21, 2024
A stroke affects the brain’s arteries and occurs when a blood vessel that brings blood to the brain gets blocked or ruptures. The area of the brain that is supplied with blood by the blocked or ruptured blood vessel doesn’t get the oxygen and nutrients it needs, and without oxygen, nerve cells are unable to function. Since the brain controls one’s ability to move, feel, and think, a stroke can cause injury to the brain that could affect any or all of these functions.
Everyone should know the signs of a stroke and seek immediate medical attention if you think you or someone around you is having a stroke. If you or someone you love has recently had a stroke, then it’s important to understand what happens next.
Know the Symptoms of a Stroke and act FAST
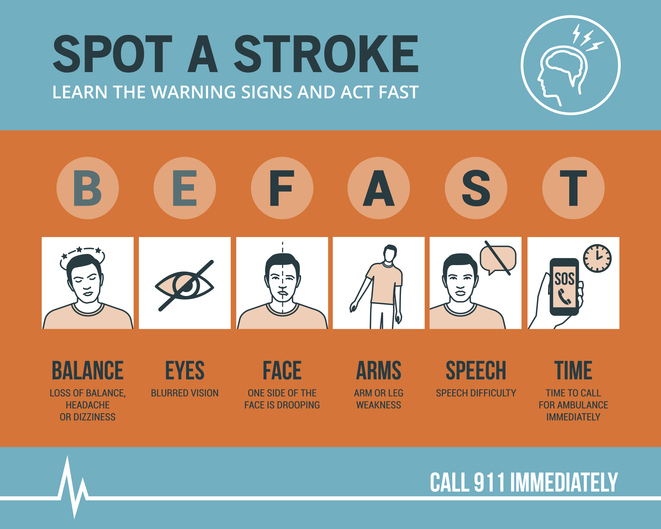
The longer the brain is left untreated during a stroke, the more likely it is that someone will have irreversible brain damage. The acronym FAST can help everyone recognize the four main signs that someone may be having a stroke and remember to act fast in seeking medical treatment. That means calling 9-1-1 immediately, as emergency response workers can treat someone on arrival if they think that person is having a stroke.
FAST stands for Facial drooping, Arm weakness, Speech difficulties, and most importantly, Time. If one side of a person’s face is drooping, if the person cannot lift both arms or one arm is drifting downward, and if the person’s speech is slurred or they cannot repeat a simple sentence, then they may be having a stroke. Not all of these signs need to be present to signal a stroke. Just one or two of these symptoms is enough to call 9-1-1, because time is of the essence in the event of a stroke.
Stroke Treatment Begins With Emergency Response Workers
Calling for an ambulance means that the emergency response workers can start life-saving treatment on the way to the hospital. Stroke patients who are taken to the hospital in an ambulance may get diagnosed and treated more quickly than people who wait to drive themselves. The emergency workers may also know best where to take someone, such as to a specialized stroke center to ensure that they receive the quickest possible treatment. The emergency workers can also collect valuable information for the hospital medical staff before the patient even gets to the emergency room, alerting staff of your arrival and allowing time to prepare. All of what the ambulance team can provide saves time in the treatment of stroke, and in the event of a stroke, time is of the essence.
Ischemic Stroke or Hemorrhagic Stroke?
There are two different kinds of stroke, ischemic or hemorrhagic. A medical team will need to determine which kind of stroke the patient is having in order to direct treatment. An ischemic stroke accounts for 87% of all strokes and happens when a blood clot blocks a vessel supplying blood to the brain. Hemorrhagic stroke happens when a blood vessel ruptures and bleeds within or around the brain.
“Fifty percent of strokes present with a clot in a large vessel in the brain, and these don’t respond very well to the old treatment, the IV clot busting medicine,” says M.D. and director of the Sparrow Comprehensive Stroke Center Anmar Razak. “And so nowadays, we do surgery, and what we do is we rush them into the hospital, into the cath lab. We quickly get access through the blood vessels and get up to where the clot is and pull it out.”
With ischemic stroke, the treatment goal is to dissolve or remove the clot. A medication called alteplase or tPA is often administered and works to dissolve the clot and enable blood flow. Alteplase saves lives and reduces the long-term effects of a stroke but must be given to the patient within three hours of the start of a stroke. Then, a procedure called mechanical thrombectomy removes the clot and must happen within six to 24 hours of stroke symptom onset.
For hemorrhagic stroke, the treatment goal is to stop the bleeding. There is a less-invasive endovascular procedure involving a catheter being threaded through a major artery in an arm or leg toward the area of the bleeding in the brain where a mechanism is inserted to prevent further rupture. In some cases, surgery is required to secure the blood vessel that has ruptured at the base of the bleeding.
Rehabilitation After a Stroke
Perhaps the most important part of stroke treatment is determining why it happened or the underlying causes of the stroke. Stroke risk factors include high blood pressure, which weakens arteries over time, smoking, diabetes, high cholesterol, physical inactivity, being overweight, heart disease including atrial fibrillation or aFib, excessive alcohol intake or illegal drug use, and sleep apnea. By making the right lifestyle choices and having a good medical management plan moving forward, the risk of another stroke can be greatly reduced.
That’s because if you have had a stroke, you are at high risk for having another one. One in four stroke survivors have another within five years, while the risk of stroke within 90 days of transient ischemic attack or TIA is as high as 17% with the greatest risk during the first week. This is why it becomes so important to determine the underlying causes of the initial stroke. Your doctor may give you medications to manage a condition, such as high blood pressure, and then recommend lifestyle changes, including a different diet and regular exercise.
Rehabilitation after a stroke begins in the hospital, often within only a day or 2 after the stroke. “There are so many things that patients need to fall into place to be functional and independent again after a stroke,” said Razak. “And they always come down to speed and time.” Rehabilitation can help with the transition from the hospital to home and can help prevent another stroke. Recovery time after a stroke is different for everyone and can take weeks, months, or even years. Some people may recover fully, while others may have long-term or lifelong disabilities. Stroke rehabilitation should be thought of as a balance between full recovery and learning how to live most effectively with some deficits that may not be recovered.
Difficulties from a stroke range from paralysis or weakness on one or both sides of the body, fatigue, trouble with cognitive functioning such as thinking and memory, seizures, and mental health issues like depression or anxiety from the fear of having another stroke. Everyone’s rehabilitation will look different based on their difficulties after a stroke but may include speech, physical, and occupational therapy. Speech therapy helps when someone is having problems producing or understanding speech, physical therapy uses exercises that help someone relearn movement and coordination skills, and occupational therapy focuses on improving daily activities, such as eating, dressing, and bathing. Joining a patient support group may help people adjust to life after a stroke, while support from family and friends can also help relieve the depression and anxiety following a stroke. It’s important for stroke patients to let their medical team and loved ones know how they’re feeling throughout their recovery and what they may need help with.
Stroke rehabilitation can be hard work, but just as in the initial treatment of a stroke, time matters in the possibility of a full recovery. Many survivors will tell you that rehabilitation is worth it and recommend using motivators to achieve recovery goals, such as wanting to see a child’s graduation or returning to working in the garden. With Insureyouknow.org, caretakers may keep track of medical treatments and rehabilitation plans in one easy-to-review place so that they may focus on caring for their loved one during the period of recovery from stroke.
May is American Stroke Month which aims to raise awareness of the second leading cause of death.
Gardening for Mental Well-Being
May 15, 2024

Interest in gardening has increased since the pandemic, as more and more people are searching for ways to disconnect from stressful times and reconnect to nature. It turns out that immersing ourselves in green spaces and caring for plants is a form of caring for ourselves. Time spent in nature has been found to improve mental health so much so that gardening has been prescribed by the National Health Service in Great Britain since 2019. But while scientists are just beginning to pay attention to nature’s overall effect on our health, humans have known about the power of gardening for a very long time.
Historic Gardens and Horticultural Therapy
Ancient and modern gardens all over the world, including Persian pleasure gardens, Islamic paradise gardens, Chinese courtyard gardens and Japanese rock gardens, nurture a sense of separation from the chaotic world and provide a place for inward reflection. In addition to sources of food, the Roman Empire treated gardens as a place to cultivate mindfulness. As extensions of the home, Roman gardens were the first outdoor rooms. They served as spaces to rest and marvel at nature’s wonder. By the Middle Ages, hospital gardens modeled after these Roman gardens were seen as integral parts of the hospital, not just to feed patients and grow medicines but to offer patients time outside. But as efficiency and technology took over medical treatment, these spaces went extinct.
Still, the benefits of gardens were not forgotten. In the 1800s, early American psychiatrists began noting links between horticulture and mental health. Born in 1933, the famous neurologist Dr. Oliver Sacks believed that gardens and nature were more powerful than any medication. As the scientific evidence of spending time in green spaces leading to better health grew, many hospitals began incorporating gardens into their facilities again and horticultural therapy was developed as a therapeutic practice in the 1970s.
Horticultural therapy involves taking care of plants with specific goals for the patient in mind. For instance, tending to a garden and watching it thrive can help people build self-esteem and feel a sense of accomplishment. Gardening can also lead to life lessons, such as when a plant dies, the person can ask themselves, “What could I have done differently?” Connecting the garden to themself can lead them to think that maybe they can do a little more to take care of themself, too. “It’s really the plants that are the therapists,” says Laura Rumpf, a horticultural therapist who treats patients with dementia through gardening. “Even if somebody can’t necessarily name what it is they’re smelling, the body somehow remembers.” For those with dementia for instance, plants can help them to reminisce which leads to telling stories and sharing memories, an important part of connecting to others and validating their identity.
The Scientific Proof of Nature’s Benefits
Gardening involves exercise, which we know is beneficial to our health, and since people tend to breathe more deeply when they’re outside, outdoor activities can clear the lungs, aid digestion, and improve immune responses. Sunlight also lowers blood pressure and increases vitamin D levels, but the benefits of outdoor gardening extend beyond these physical benefits.
A recent study conducted by scientists at the University of Florida found that gardening lowered stress, anxiety and depression in healthy women who attended a gardening class twice a week. “Past studies have shown that gardening can help improve the mental health of people who have existing medical conditions or challenges,” said the principal investigator of the study Charles Guy. “Our study shows that healthy people can also experience a boost in mental well-being through gardening.” In addition to improved mental well-being, interacting with nature has proven cognitive benefits. A 2019 study by University of Chicago psychologist Marc Berman showed that green spaces near schools promote cognitive development in children, while adults assigned to public housing in green neighborhoods exhibited better attentional functioning than those assigned to units with less access to green spaces.
Scientists have a few ideas as to why nature is so good for our mental health. One hypothesis is that since our ancestors evolved in the wild and relied on their environment for survival, we have an innate drive to connect with nature. As a species, we may be attracted to plants because we depend on them for food and shelter. Another hypothesis is that spending time in nature triggers a physiological response that lowers stress levels. Throughout human history, trees and water have been an oasis and signaled relaxation. There is an implicit trust in nature that calms our parasympathetic nervous system. Yet a third hypothesis is that nature replenishes cognitive functioning, which restores the ability to concentrate and pay attention. The truth probably lies in a combination of all of these theories.
Gardening Against Loneliness
Perhaps one of the most overlooked yet obvious benefits of gardening is that it can make people feel less alone in the world. While gardening can bring people together through community gardens, one doesn’t even need to be around other people while spending time in nature in order to feel more connected to others. “Nature can be a way to induce awe,” said psychology professor John Zelenski. “One of the things that may come from awe is the feeling that the individual is part of a much bigger whole.”
Gardening can bring people together through a sense of community, as people who garden are rich with expertise that they are willing to share with other gardeners. Master gardeners and local volunteers dedicate their time to empowering other people in the community who are interested in growing their own plants. Simply sharing a gardening blunder is just one way to connect with a fellow gardener. Social connections are important for our mental well-being because they help lower stress, improve resilience, and provide support, while a strong sense of belonging has been shown to lower one’s risk of depression and anxiety.
Community gardens are a great place to connect with others as they offer room for talking during uncomplicated and repetitive tasks. Since gardening can bring together all kinds of people, time in the garden with others can also remind us that we are more alike than not. “Gardens are a great point of connection,” said the director of a London community garden Sarah Alun-Jones. “We often find ourselves talking about where we grew up, our childhood gardens, food we like to grow and cook… and we learn lots along the way.”
If you’re thinking of incorporating gardening into your routine, it doesn’t need to be intimidating. Simply starting by potting indoor plants or taking walks in green spaces during your lunch break are just two simple ways to connect with nature now. At Insureyouknow.org, you may store all of your gardening plans and records, so that you can become the researcher of your own gardening benefits.
