Tag: Inflation Reduction Act
Medicare Will Cover Shingles Vaccine in 2023
December 27, 2022
Starting in January 2023, Medicare will cover the cost of the shingles vaccine, Shingrix.
The Centers for Disease Control and Prevention (CDC) recommends adults 50 years and older get two doses of Shingrix two to six months apart to prevent complications from the disease shingles. Shingrix is more than 90 percent effective in preventing illness, according to the CDC. But for many people on Medicare, it had been unaffordable at more than $200 for the shot regimen.
The Inflation Reduction Act of 2022 aims to reduce the cost of some drugs and close this barrier to good healthcare. As of January 2023, all vaccinations covered under Medicare part D that are approved and recommended by the Centers for Medicare and Medicaid and the CDC will be covered without a copay. So, no cost-sharing will be associated with the administration of Shingrix, as well as flu shots; tetanus, diphtheria, and pertussis vaccines; and COVID-19 vaccines.
What is “shingles”?
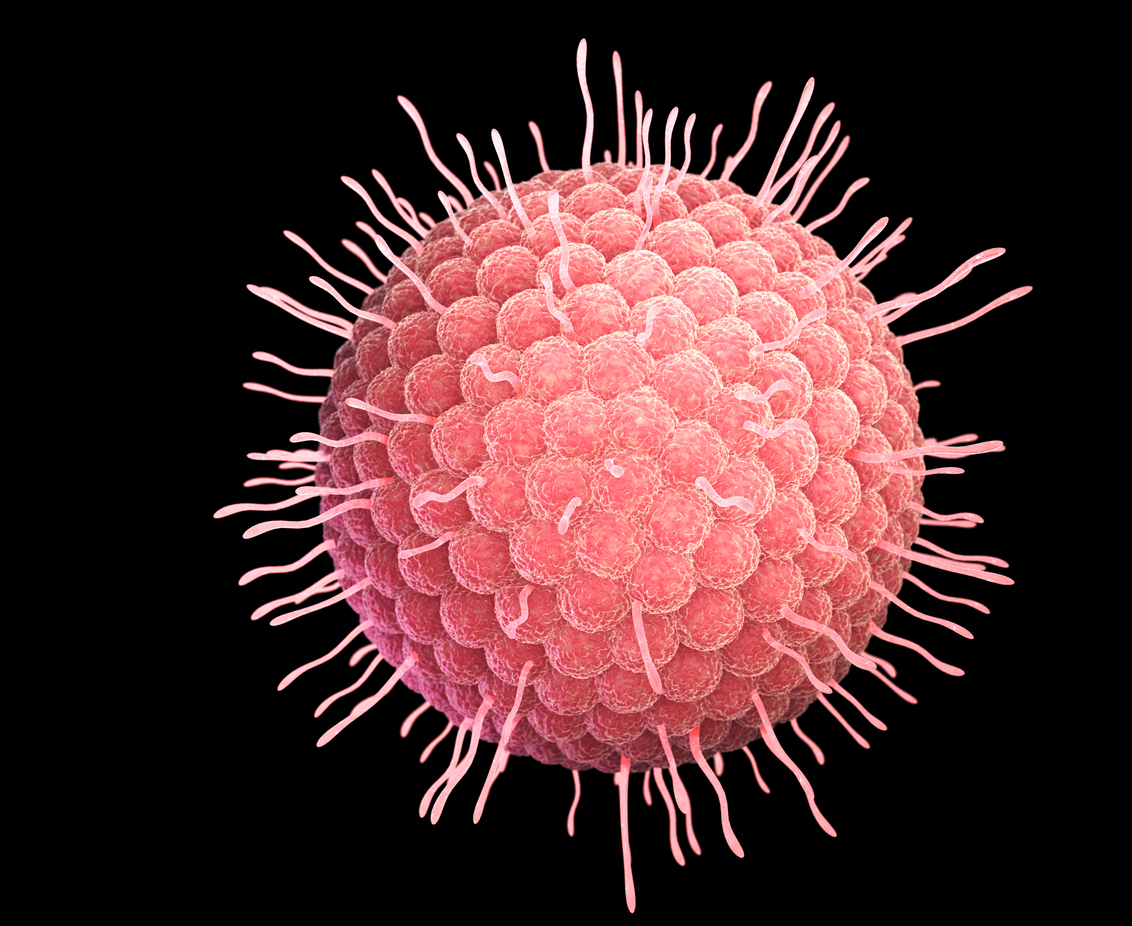
Shingles is an invasive, painful outbreak of rash or blisters on the skin that can damage your vision or hearing, make you lose hair, and cause long-term nerve pain. It is caused by the varicella-zoster virus—the same virus that erupts in chickenpox. After you have chickenpox, the virus stays in your body. It may not result in problems for many years, but as you get older, the virus may reappear as shingles.
Is shingles contagious?
Shingles is not contagious. But you can catch chickenpox from someone with shingles. If you’ve never had chickenpox or the chickenpox vaccine, try to stay away from anyone who has shingles. If you have shingles, try to stay away from anyone who has not had chickenpox or the chickenpox vaccine, or anyone who might have a weak immune system.
Who is at risk for shingles?
Anyone who has had chickenpox is at risk of getting shingles. More than 99 percent of Americans born before 1980 have had chickenpox, even if they don’t remember it. The risk of contracting shingles increases as you get older; shingles is most common in people over 50. People with weakened immune systems are at higher risk of getting shingles. About one out of every three people in the United States will develop shingles during their lifetime. It is rare, but possible, to get shingles more than once.
What are the symptoms of shingles?
Early signs of shingles include burning or shooting pain and tingling or itching. It is usually on one side of the body or face. The pain can be mild to severe.
One to 14 days later, you will get a rash. It consists of blisters that typically scab over in 7 to 10 days. The rash is usually a single stripe around either the left or the right side of the body. In other cases, the rash occurs on one side of the face. In rare cases (usually among people with weakened immune systems), the rash may be more widespread and look like a chickenpox rash. Some people may also have other symptoms, including fever, headache, chills, and an upset stomach.
What are some complications caused by shingles?
- Postherpetic neuralgia (PHN) is the most common complication of shingles. It causes severe pain in the areas where you had the shingles rash. It usually gets better in a few weeks or months, but some people can have pain from PHN for many years, and it can interfere with daily life.
- Temporary or permanent vision loss can happen if shingles affects your eye.
- Hearing or balance problems are possible if you have shingles within or near your ear. You may also have temporary or permanent weakness in the muscles on that side of your face.
- Very rarely, shingles can also lead to pneumonia, brain inflammation (encephalitis), or death.
How is shingles diagnosed?
Usually, your healthcare provider can diagnose shingles by taking your medical history, looking at your rash, and after scraping off tissue from the rash or swabbing some fluid from the blisters, sending the sample to a lab for testing.
How can shingles be treated?
There is no cure for shingles. Antiviral medicines may help make the attack shorter and less severe. They may also help prevent PHN. Recommended medicines are most effective if you can take them within three days after the rash appears. Pain relievers may also help with the pain. A cool washcloth, calamine lotion, and oatmeal baths may help relieve some of the itching associated with shingles.
InsureYouKnow.org
If you are at risk of getting shingles, contact your healthcare provider or pharmacist to schedule a Shingrix shot early in 2023, even if you are not covered by Medicare. Shingrix is also covered by most health insurance plans so check with your insurance provider to see if the vaccine is included in your plan.
At insureyouknow.org, record the date of your first shot and set a reminder for your second shot two to six months later. You’ll be off to a great start in preventing the pain and possible side effects of shingles in 2023.
Kick Your Health Benefits into High Gear
December 1, 2022

As open enrollment season kicks into high gear, millions of people will have an opportunity to choose their 2023 health benefits.
Employers’ Healthcare Costs
Employers’ healthcare costs are rising, with large companies forecasting up to an 8 percent increase for 2023. The main difference with previous years will be higher prescription drug costs, which will jump 10 percent, the highest in the past decade.
Many companies will try to limit the share they pass along to their workers, as benefits are seen as a key attraction and retention tool in a tight job market.
Employees’ Healthcare Costs
For 2022, annual family premiums for employer-sponsored health insurance averaged $22,463, up slightly from $22,221 in 2021, according to the 2022 benchmark KFF Employer Health Benefits Survey. On average, workers contributed $6,106 toward the cost of family premiums, with employers paying the rest. The average premium for single coverage was $7,911 (up from $7,739 in 2021), with employees paying $1,327 annually, according to the survey. Nine percent of covered workers, including 21 percent of covered workers at small firms, are in a plan with a worker contribution of $12,000 or more for family coverage.
While premium data for 2023 generally won’t be available until after the new year begins, workers may see larger increases than in recent years.
Triple-Tax Advantaged HSAs
Some tools can help you manage your healthcare costs. More than three-quarters of large employers offer Health Savings Accounts (HSAs) that offer triple tax advantages: money contributed is pre-tax, it grows on a tax-free basis, and then can be withdrawn tax-free to pay for qualifying medical expenses now or in the future, all the way through retirement.
You can contribute to an HSA only if you’re enrolled in a qualifying high-deductible health plan. Average annual premiums for workers enrolled in HSA plans are lower than the overall average, but workers shoulder higher costs until they meet their deductible.
Employees can contribute up to $3,850 to their HSA for individual coverage for 2023, up from $3,650 this year; for family coverage, workers can contribute up to $7,750, up from $7,300 this year, per an announcement by the Internal Revenue Service. Catch-up contributions for those 55 and over remain $1,000.
Many HSAs give account holders the option to invest a portion of their money in the stock market. But fewer than 10 percent do so, as opposed to leaving their money just sitting in cash. If you can afford to pay your medical bills through your regular cash flow, your HSA funds will likely grow over time in the market and can be used in retirement to pay for a range of qualifying medical expenses.
HSAs are portable and remain with the owner through plan and job changes. If you are no longer enrolled in a qualifying high-deductible health plan, you can no longer contribute to your account, but you can still tap it to pay qualifying medical costs. Flexible-spending accounts (FSAs), by contrast, are linked to a particular employer; unlike HSA funds, money in an FSA must be spent down or forfeited within a certain period.
Health Insurance Plans under the Affordable Care Act
Outside of the employer market, open enrollment began on November 1 on Healthcare.gov for individual and family health insurance plans under the Affordable Care Act. In most states, open enrollment ends on January 15, although you must enroll by December 15 if you want coverage to begin on January 1. The Inflation Reduction Act extended the enhanced premium subsidies for ACA enrollees through 2025; for many, that may offset the moderate average increases expected to premiums.
Impact of Rising Drug Costs
There are two main reasons drug costs are rising: First, pharmaceutical companies are introducing better, but more expensive drugs for several important conditions. In most years, total drug cost would be tempered by other brand name drugs that were being replaced by generics, but in 2023, there will be fewer of these than usual.
Second, pharmaceutical companies are raising the prices they charge to private health insurance plans because they anticipate having to lower the prices they charge to Medicare. The recent Inflation Reduction Act allows Medicare to negotiate drug prices for the first time. Currently, only 10 drugs are on the negotiation list, but these are widely used. The list will rise to 20 drugs in the future.
The “No Surprises” Act
The “No Surprises” Act that went into effect in January 2022 is having its intended effect of lowering surprise out-of-network charges to patients who get emergency care, non-emergency care from out-of-network providers at in-network facilities, and air ambulance services from out-of-network providers.
InsureYouKnow.org
After you determine your healthcare insurance coverage for 2023, file your decisions at insureyouknow.org. Keep aware of government mandates that can affect your healthcare expenses for prescription drugs, out-of-network charges, changes in Medicare, increases in premiums, and your HSA and FSA contributions and withdrawals.
