Category: Health
Medical ID Wallet Cards vs. Digital Access: Which is Better?
February 11, 2026

The Emergency Question
Picture someone collapsing in a store, unable to talk. Paramedics rush over but need answers. What allergies does this person have? What medications? Any serious health problems? Should these details live on a card in their wallet or sit on their phone?
Here’s the thing: picking just one isn’t the best move.
Medical ID Wallet Cards
Advantages
- Battery? What battery? These cards just work, period.
- First responders get it: About 95% of EMTs know to check wallets.
- Zero connectivity needed: Mountains, basements, middle of nowhere. Doesn’t matter.
- Won’t break the bank: Spend maybe $5-10 once, that’s it.
Disadvantages
- There’s only so much room on a tiny card.
- Wallets get misplaced or left at home sometimes.
- People forget to scratch out old info and add new stuff.
- Cards get wet, fade, or become hard to read after a while.
Digital Smartphone Medical IDs
Advantages
- Room for everything: Write down every single medication and condition.
- Updates take two seconds: New prescription? Changed doctors? Fixed instantly.
- Talks to 911: iPhones automatically send this stuff when someone dials emergency.
- Costs nothing: Already sitting in the phone waiting to be used.
Disadvantages
- Dead phone equals zero help.
- Some paramedics haven’t learned the tricks for every phone type yet.
- Accidents crack screens and destroy phones pretty often.
- Weird fact: Only about 1 in 4 people actually bother setting this up.
The Smart Choice: Use Both
- Medical Alert Jewelry: Get a bracelet stamped with the biggest health concern plus “SEE WALLET CARD”.
- Wallet Card: The most important stuff, right there in physical form.
- Digital Medical ID: Everything else stored on the phone (make sure it shows without unlocking).
- Backup Copies: Stick extras in the glove box, desk drawer, with Mom or a close friend. Consider using a secure digital vault like InsureYouKnow to store copies of medical cards, insurance information, and emergency contacts that family members can access when needed.
Quick Setup
Wallet Card:
- Write down allergies, health conditions, meds, who to call.
- Get it laminated so it lasts.
- Make a few copies.
iPhone:
- Open Health app → Find Medical ID → Turn on “Show When Locked”.
Android:
- Go to Settings → Look for Safety & Emergency → Switch on “Show on Lock Screen”.
Total time needed: about 10 minutes.
Real Examples
- Diabetic collapse: Woman’s wallet card listed her insulin information. Paramedics knew exactly what to do.
- Allergic reaction: Guy’s phone shattered during his fall. Good thing his wallet card mentioned that penicillin allergy.
- Lost senior: Older woman wandered off, couldn’t remember her name. Her iPhone Medical ID had her daughter’s number right there.
Who Needs This?
People dealing with:
- Health stuff like diabetes, seizures, heart trouble.
- Bad allergies that could turn dangerous.
- Pills they take every day.
- Pacemakers, implants, that kind of thing.
Common Mistakes
- Picking one method and ignoring the other.
- Setting it up once and never looking at it again.
- Leaving the lock screen access turned off on phones.
- Keeping it secret from family members.
The Bottom Line
Why choose? Wallet cards save the day when phones quit. Digital files hold way more detail than any card could. Together, they’ve got each other’s backs.
- Money spent: Less than fifty bucks
- Time invested: Ten minutes
- Potential payoff: Might literally save someone’s life
Action Steps
- Today: Get that phone Medical ID set up (takes 5 minutes).
- This week: Print out a wallet card (another 5 minutes).
- Twice a year: Check both and update anything that changed.
When things go wrong, having a backup plan makes all the difference.
Storing Everything Securely
Beyond wallet cards and phone apps, keeping digital copies of medical information in a secure vault ensures family members can access critical details during emergencies. Platforms like InsureYouKnow provide encrypted storage for medical records, insurance policies, medication lists, and emergency contacts. This creates another layer of protection, especially when someone needs to share information with multiple family members or caregivers.
Medical History Cheat Sheet: What ER Doctors Need
February 4, 2026
The “Golden Hour” Gap
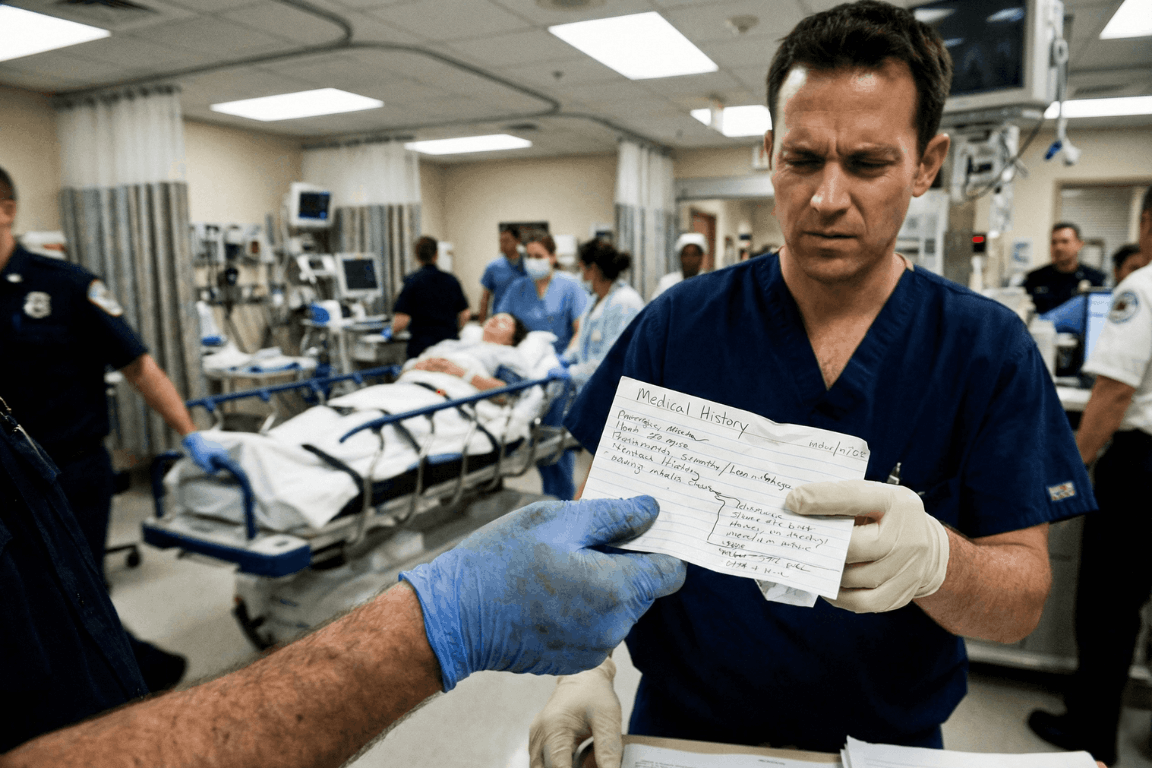
The Emergency Room is a storm. Noise. Chaos. Speed. Doctors and nurses fight the clock. They chase the “Golden Hour.” That tiny window where fast action beats death.
But silence is the enemy. Ambulances dump patients who can’t talk. Shock takes over. Or they are out cold. In that high-pressure moment, a missing detail, a drug allergy, an old surgery, sends the team down the wrong road. That road ends badly.
Ask any ER staffer. They agree on one thing. A simple “cheat sheet” is the best tool a person can bring through those doors.
Why Memory Fails in a Crisis
People think they will remember. “I know my meds,” they say. They are wrong. Trauma wipes the brain clean. Pain and fear take over. A patient knows they take a “heart pill.” The name? Gone. The dose? Forgotten.
A written paper fixes this. It talks when the mouth cannot. It stops the guessing game between a frantic arrival and safe care.
The ER Doctor’s Wish List: 6 Essentials
What goes on the paper? Forget the thick file. Medical teams want facts. Facts that change the plan right now.
1. The “Big Picture” Demographics
Before the IV goes in, the team must know who they are treating. They need to know who signs the forms.
- Full Legal Name and Date of Birth: This finds old records in the computer.
- Blood Type: Vital for fast transfusions.
- Emergency Contacts: A spouse. A parent. Someone who answers “yes” or “no” to surgery when the patient can’t.
2. The Medication List (Crucial)
This part kills people if it’s wrong. Drug interactions cause huge messes in hospitals. Be exact:
- Prescription Drugs: The name. The dose (like 50mg). The schedule.
- Over-the-Counter (OTC) Meds: Aspirin. Ibuprofen. They seem safe. They aren’t. They thin blood. They hit kidneys.
- Supplements and Vitamins: Herbal pills often fight with anesthesia.
Note: Never write “Take as directed.” That tells the doctor zero.
3. The Allergy Alert
Does the patient hate penicillin? Latex? Contrast dye? The team needs to know. Now. The wrong drug turns a broken bone into a breathing emergency. List the allergen and the reaction. “Penicillin: Hives.” “Peanuts: Throat shuts.”
4. Past Medical History (PMH)
Context is king. A stomach ache in a healthy teen is one thing. In a Crohn’s patient, it’s another.
- Chronic Conditions: Diabetes. Asthma. Epilepsy. High blood pressure. Heart issues.
- Implants: Pacemakers. Metal rods. Artificial joints. The team must know this before an MRI scan starts.
- Past Surgeries: A quick list. “Appendectomy, 2015.” “C-Section, 2020.”
5. Recent History
Sometimes the clue is new. A note about travel, especially overseas, helps. So does a note about recent hospital stays. This helps doctors spot weird infections.
6. Insurance and Directives
Life comes first. But paperwork causes headaches later. List Insurance Policy and Group Numbers. Also, check for an Advance Directive or DNR (Do Not Resuscitate) order. A copy must exist. Otherwise, the patient’s wishes get ignored.
Paper vs. Digital: The Accessibility Problem
Old advice? Keep a card in a wallet. But paper sucks. It fades. It tears. It gets lost. Or it sits in a kitchen drawer while the car crash happens three towns over.
Digital vaults like InsureYouKnow.org changed the game. Storing this “Cheat Sheet” in a secure cloud keeps data safe. It stays ready. A trusted partner pulls up the vault on a phone. Seconds later, the ER team has the facts.
The Final Diagnosis
Being ready isn’t paranoia. It is smart. A Medical History Cheat Sheet takes ten minutes. It pays off in safety. It lets doctors work faster. It stops bad errors. And it gives families peace. They know the health story is clear. Even when the room is silent.
Sandwich Generation Guide: Organize Parents’ & Kids’ Records
January 8, 2026
The Squeeze is Real
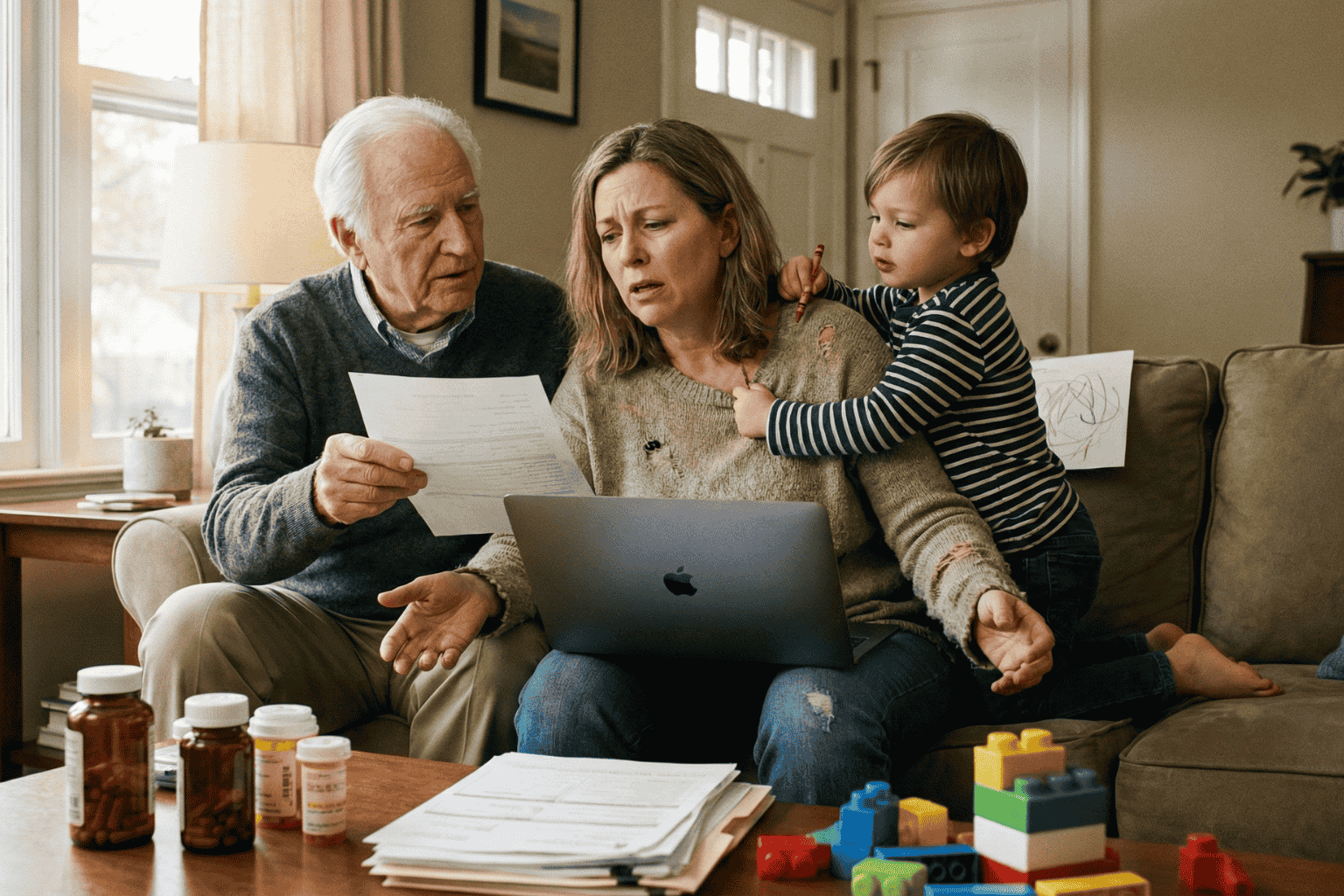
The term “Sandwich Generation” sounds polite, almost clinical. But for the millions of adults living it, the reality feels a lot more like a pressure cooker. They are squeezed tight. On one side, there are children needing help with homework, permission slips, and growing pains. On the other, aging parents need support with doctors, medications, and a lifetime of accumulated paperwork.
It is exhausting.
The hardest part usually isn’t the physical caregiving. It is the administration. It is being the unpaid, overworked secretary for two different households. One minute, a parent is hunting for a vaccination card for summer camp; the next, they are frantically searching for Mom’s Medicare supplement number because a receptionist is waiting on the line.
When these worlds collide, chaos wins. Unless, of course, there is a system in place.
Two Households, One Overloaded Brain
The main problem isn’t a lack of effort. It is a lack of centralization. The “Sandwich” caregiver is trying to run two different operating systems at once.
Consider the children. Their documentation is constant and urgent:
- Social Security cards (usually lost in a drawer somewhere).
- Immunization records that schools demand every September.
- Birth certificates for sports or travel.
Then look at the parents. Their paper trail is decades long and much heavier:
- Wills, Trusts, and Deeds (often hidden in “safe” places that no one can find).
- Complex lists of daily medications.
- Insurance policies that need to be renewed.
- The dreaded “In Case of Emergency” contacts.
Keeping the kids’ files in a backpack and the parents’ files in a dusty filing cabinet across town simply doesn’t work. Not in 2026. When an emergency happens, and they always happen at inconvenient times, nobody wants to be driving across town to find a piece of paper.
The “Kitchen Table” Talk
Getting organized starts with a conversation, not a scanner. This is the tricky part. Many adults feel awkward asking their parents about wills or bank accounts. It feels intrusive.
But the conversation doesn’t have to be about control. It should be about safety. The approach matters. Framing it as, “We need to make sure the doctors know what you need if you can’t tell them,” works a lot better than, “Give me your passwords.”
The goal is strictly practical: preventing a crisis from becoming a disaster.
Cut the Clutter: What Actually Matters?
A common mistake is trying to save everything. But honestly, nobody needs to digitize a utility bill from 1998. To survive the squeeze, caregivers need to be ruthless about what they keep.
The “Must-Have” list is actually quite short:
- The Legal Shield: Power of Attorney. This is non-negotiable. Without it, an adult child is legally a stranger to their parent’s bank or doctor.
- The Medical Snapshot: A simple, updated list of what pills they take and who their primary doctor is.
- The Money Trail: Just a list of where the accounts are. Not necessarily the balances, but the locations of the banks and insurance policies.
Stop Relying on Physical Folders
Paper is fragile. It burns, it tears, and most importantly, it stays in one place.
If a parent falls ill while the caregiver is on vacation, that physical folder in the hallway closet is useless. This is why moving to a digital system is the only logical step for a modern family.
Using a secure, encrypted platform, like InsureYouKnow.org, solves the geography problem. It puts the information in the cloud, protected by encryption that is tougher than any lock on a filing cabinet. It means the right information is available on a smartphone, right in the hospital lobby, exactly when it is needed.
Don’t Go It Alone
There is a hero complex in the Sandwich Generation. Everyone tries to carry the load solo. But that is a recipe for burnout.
Once the records are digital, they should be shared. A spouse, a reliable sibling, or a family attorney needs access, too. Modern digital vaults allow for this kind of “trusted partner” access. It ensures that if the primary caregiver gets the flu or gets stuck in a meeting, someone else can step in and handle the situation.
Finding Some Peace
At the end of the day, organizing these records isn’t really about paperwork. It is about buying back time.
Every minute saved by not hunting for a lost insurance card is a minute that can be spent actually being a parent or a son or daughter. The paperwork will always be there, but the stress doesn’t have to be. By merging these two chaotic worlds into one secure place, the Sandwich Generation can finally take a breath.
5 Scams Targeting Seniors in 2026 (And How to Lock Down Your Data)
January 1, 2026
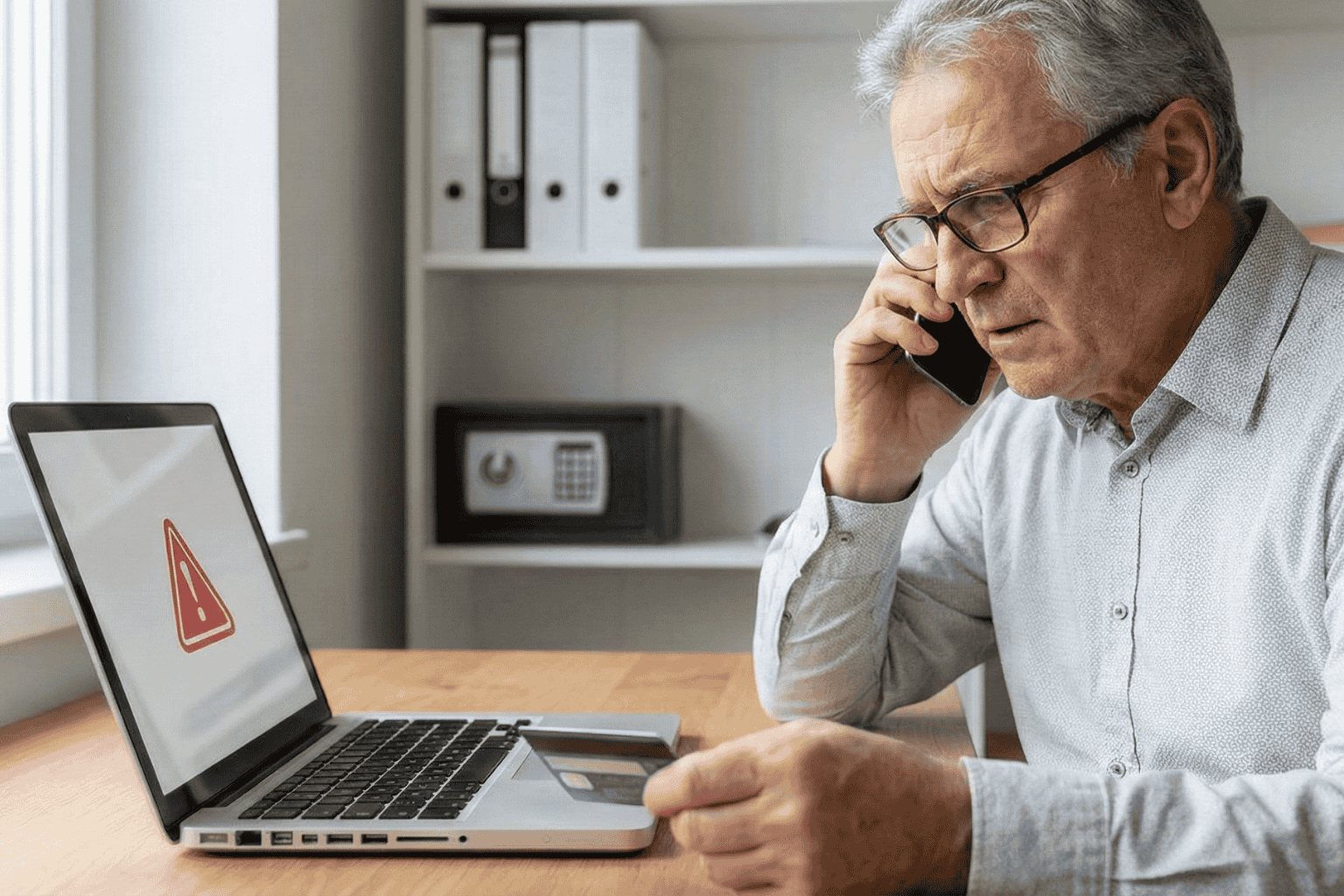
Can you believe it is 2026? We have apps for everything and phones that are smarter than the computers we grew up with. But there is a flip side. All this tech has handed crooks a brand new playbook. And let’s be honest, they love targeting seniors.
The scams floating around right now aren’t the sloppy emails we used to laugh at. These new ones are sharp. They use fancy tech and psychological tricks to bypass your gut instincts. But don’t worry. You don’t need to be a tech wizard to stay safe; you just need to know what the red flags look like.
Here is what is happening out there and how to keep your private life private.
1. The “Grandchild” Voice Clone (It’s Not Them)
You might remember the old version of this trick. Someone calls pretending to be a grandson in trouble. Usually, you could tell it wasn’t him because the voice was off.
Well, the game has changed.
Scammers are now grabbing snippets of audio from social media videos. If your grandchild posted a video on TikTok or Instagram, that is all they need. They use AI to clone the voice. When the phone rings, it sounds exactly like them. Same laugh, same tone. They will say they are in jail or stuck in Mexico and need money fast.
What to do:
- The Password Rule: Agree on a secret family password. If “Bobby” calls saying he is in trouble, ask for the password. If he can’t give it, hang up.
- Don’t Panic: Hang up and call their real cell phone number. Verify it yourself.
2. The “Computer Meltdown” Pop up
You are just reading the news or looking for a recipe, and suddenly BAM. A siren starts wailing from your speakers. A box pops up on the screen saying your computer is infected and you have to call “Microsoft” immediately.
It is terrifying, right? That is the point.
But here is the truth. It is all smoke and mirrors. Your computer is fine. The person on that phone line isn’t tech support; they are a thief waiting for you to open the front door. If you let them “remote in,” they will swipe your passwords or charge you for fixing a problem that didn’t exist.
What to do:
- Ignore the Number: Real companies like Apple or Microsoft will never put a phone number on a warning pop up. Never.
- The Hard Reset: If your mouse freezes, just hold the power button down until the screen goes black. Turn it back on, and the “virus” will be gone.
3. The Medicare “Chip Card” Trap
Medicare rules are a maze, and scammers know it. The latest trick? A friendly phone call telling you that you are due for a “refund” or a new “chip card.”
It sounds great, doesn’t it? But then comes the catch. To get the goods, they say they just need to “verify” your Social Security Number or your current Medicare ID.
What to do:
- Guard It: Treat your Medicare number like the combination to a safe.
- Check Your Vault: Don’t take a stranger’s word for it. If you keep your insurance details stored in a secure spot, like the InsureYouKnow.org portal, you can just log in and check your official policy. Call the number on your documents, not the one the stranger gave you.
4. The “Pig Butchering” Long Game
This one is nasty because it pulls on heartstrings. It usually starts with a “wrong number” text or a random message on Facebook. The person is nice. You start chatting. Over weeks, maybe even months, you become friends.
Then, they mention money. They are making a killing in crypto or gold, and they want to help you do the same. You might even put a little money in and see it grow on a website they send you. But the moment you invest a serious amount? The website vanishes, and so does your “friend.”
What to do:
- Keep Wallets Closed: Never take financial advice from someone you have only met through a screen.
- Do Your Homework: If they send a photo, run it through a Google Image search. You will probably find that picture belongs to a model or someone else entirely.
5. The Fake Government Threat
Fear is a powerful tool. Scammers love to pretend they are the IRS or the Social Security Administration. You will get a text or voicemail saying your account is “suspended” or you owe back taxes.
They will threaten arrest if you don’t pay right now. And weirdly, they often want payment in gift cards.
What to do:
- Gift Cards equal Scam: The government will never ask you to pay a fine with an Amazon gift card. That just doesn’t happen.
- Slow Down: They want you to panic so you stop thinking. Take a breath. It is almost certainly fake.
The Secret Weapon? Getting Organized.
Why do these scams work? Because they rely on chaos. They hope you don’t know where your real policy is. They hope you can’t find the right phone number to check if the story is true.
If you have your house in order, they can’t touch you.
When you have your vital info, like IDs, policies, and bank contacts, locked in a secure, encrypted hub, you have the power. If someone calls about your life insurance, you don’t have to guess. You log in, look at the real document, and you see the truth.
Stay Safe Out There:
- Verify, Verify, Verify: Don’t trust Caller ID.
- Lock It Up: Use a secure service to store your life’s paperwork.
- Buddy System: Share access to that digital vault with a family member you trust. It helps to have backup.
You don’t have to be paranoid to be safe in 2026. You just have to be organized.
Rethinking Health Resolutions for the New Year
December 31, 2025

Every January, people pledge to “eat healthier” or “exercise more,” only to see those ambitions fade by February. Traditional resolutions often focus on a narrow slice of health, like weight loss or gym check-ins, without addressing broader habits that shape long-term well-being. Instead, physicians now emphasize developing habits that improve sleep, stress management, social connection, preventive care, and daily behavior. According to the American Medical Association, health choices that fit into everyday life and provide immediate benefits are more likely to stick.
The eight unusual resolutions below reflect a broader, evidence-based view of health for 2026.
1. Cultivate a Brain Fast Before Bed
Instead of saying “get more sleep,” focus on stabilizing your sleep schedule and wind-down habits. Sleep experts recommend consistent bedtime and wake-up times. “Setting a consistent bedtime and wake time is one of the most effective changes you can make for your sleep,” says Dr. Abhinav Singh, Medical Director at the Indiana Sleep Center.
Better sleep supports cognitive function, emotional stability, and immune health, making this a resolution linked to measurable health outcomes.
2. Build a Sensory Stress-Management Plan
Stress affects both mind and body. A sensory plan that includes calming auditory or visual cues, time in natural light, and brief outdoor breaks can soften the day’s pressures. “Self-care in the form of recognizing your limits and building in even just a few minutes of time each day to recenter yourself is important,” says Dr. Joanna Bisgrove, Family Physician, Rush University Medical Center.
Acute stress relief boosts mood and productivity while protecting long-term cardiovascular health.
3. Adjust Your Environment to Make Healthy Choices Easier
Habits are easier to maintain when your environment nudges you toward them. Placing water bottles where you see them, creating a designated space for stretching, or minimizing clutter in high-stress areas all make healthy choices more automatic. Behavioral science suggests that environmental design is a powerful driver of long-term habit change, especially when willpower alone would be unreliable.
4. Prioritize Social Connection with Intent
Social connection is a proven determinant of health. People with supportive relationships experience lower stress levels and better immune responses, and strong social ties are linked to higher life satisfaction. “Self-care includes connecting with others, particularly in person if it is safe, but over the phone or internet if not,” says Dr. Bisgrove.
Make a point to plan consistent, meaningful check-ins with friends, family, or colleagues.
5. Make Mindful Eating a Daily Practice
Unlike diet rules that focus on restriction, mindful eating asks you to pay attention to hunger cues, flavor, and satisfaction. This approach reduces emotional eating and builds a healthier relationship with food without guilt.
Mindful eating supports better digestion and sustained satisfaction from meals, leading to more stable energy and fewer cravings.
6. Link Movement to Everyday Routines
A resolution to run, bike, or lift weights is excellent if you can stick to it, but many people struggle to make it part of daily life. A more approachable alternative is to link short bursts of movement to existing routines. For example, taking a walk after a meal, doing calf raises while brushing your teeth, or standing while on phone calls add meaningful activity to your day without extra planning.
7. Focus on One Low-Tech Health Habit Per Month
Rather than pursue three or five goals at once, focus on just one foundational habit per month. January might be daily hydration, February could emphasize sleep consistency, and March could focus on organizing health appointments or screenings. The American Medical Association recommends incremental goals that are specific, manageable, and tied to your daily schedule for lasting change.
8. Shape Goals Around Seasonal Needs
Health needs change with the calendar. Winter might focus on immune support and rest, while spring encourages outdoor activity and stress renewal. Aligning habits with seasonal rhythms makes resolutions feel less forced and more adaptive. Seasonal awareness helps the body and mind adjust to natural changes in daylight, temperature, and lifestyle.
Most New Year’s resolutions lose momentum because they are too broad, hard to measure, or feel disconnected from daily life. Experts advocate for specific, actionable habits that provide near-term benefits and fit into routines. Unusual resolutions invite curiosity instead of pressure. They encourage adjustment rather than perfection. This year, instead of aiming for a dramatic transformation, consider choosing habits that quietly support your health every day. Those are the changes most likely to last.
Wishing You Safe and Healthy Holiday Travels
December 1, 2025

Traveling over the holidays is an opportunity to relax and reconnect with loved ones. But traveling during peak times can also be stressful. The crowds alone can cause some anxiety and concern. Last year, more than 132 million Americans travelled for the Thanksgiving weekend. By planning ahead, you can stay safe and healthy.
A survey of Motel 6 and Studio 6 found that 51 percent of holiday travelers plan to drive, compared to 13 percent who will travel by plane. It can be both easier and more affordable to drive, but according to the U.S. Department of Homeland Security, traveling by car during the holidays has the highest fatality rate of any major form of transportation.
Traveling by Car
By taking simple precautions, drivers can keep their passengers safe. “Number one: budget in extra time,” says Vicky Nguyen, a Consumer Investigative Correspondent for the Today Show. “Even just leaving 15 minutes earlier than normal can take some of the stress out of driving in general.”
Prepare in advance by doing the following:
- Complete any necessary automotive maintenance to ensure your car is ready for the road.
- Make sure you have a full tank of gas (or a full charge for an electric vehicle) the day before you leave.
- Pack the night before and aim for 7-8 hours of sleep.
- Pack water, snacks, and medicines for every passenger, including kids and pets.
- Get comfortable by adjusting your seat and preparing your navigation system before you get going.
“It also can’t hurt to map out your route and identify rest stops, gas stations, and food options,” says Stacey Barber, vice president of AAA Travel. In the case of traffic or bad weather, build in extra time or reschedule your departure. Locate lodging along your route ahead of your trip, in case you need to stop for a night.
Your emergency essentials should include a portable cell phone charger, a first-aid kit, blankets for cold temperatures, a flashlight with extra batteries, jumper cables, and spare tires.
Follow basic driving safety guidelines, including buckling up, obeying the speed limit and other road laws, giving your full attention to the road, especially in construction zones, and avoiding distractions, such as cell phone use.
Plan to take breaks, about every two hours or 100 miles, to avoid getting sleepy on the road. Short walks and stretches during breaks can also help prevent and alleviate pain associated with prolonged sitting.
If you’re driving, keep gifts and other valuables out of sight, preferably in the trunk. At rest stops and in airports, stay alert, be aware of your surroundings, and keep your belongings close.
Traveling by Plane
If you’re flying, plan on getting to the airport two hours before your scheduled departure time. “We ask travelers to pack their patience, especially during peak travel days,” says Ha Nguyen McNeill, a TSA administrator.
Book an early flight. Flights departing after 9 a.m. are twice as likely to be delayed than those scheduled between 5-8 a.m.
Airlines are also reminding passengers to bring their Real ID, which is required for flying as of early May, and to download an airline’s app to track flight updates and receive alerts.
To avoid getting sick while flying, it’s essential to maintain a healthy diet and stay hydrated for at least a few days before traveling. Pack simple, healthy snacks, such as nuts or dried fruit, and a refillable water bottle to bring with you. Keep any necessary medicine in a carry-on so that you can access it easily.
During your flight:
- Handle your own belongings as much as possible.
- Wash your hands whenever possible with soap and water, and carry hand sanitizer and antibacterial wipes with you.
- Avoid touching your face or eyes. If you have to cough or sneeze, use a tissue.
- If you’re sick, consider postponing your trip until you recover.
No one wants to spend their vacation worrying about whether or not their house is safe. By taking basic precautions, homeowners can protect their properties from becoming easy targets of theft.
“A simple step is to lock everything. Ensure all doors, windows, and entry points are locked, including garage doors and sliding glass doors,” says Kimani George of the University of Alabama Police Department. “Secure exterior doors with sturdy deadbolt locks, and leave blinds or curtains in their usual positions. Completely closed curtains can make it obvious you’re away.”
Other steps to protect your home include the following:
- Use timers on indoor and outdoor lights to mimic a routine.
- Install visible cameras on the exterior of the home.
- Ask them to collect mail or packages (or suspend deliveries).
- Arrange for lawn maintenance to avoid the look of a vacant home
- Do not share travel plans on social media.
Announcing holiday plans or posting vacation pictures on social media puts you at a security risk. “By posting pictures of your trip on social media sites, you are alerting the public that your home is currently vacant,” says George. “It is a safer option to wait until you return home before sharing the memories of your travels.”
Holiday travel can be stressful, but being prepared can help you enjoy the time away with loved ones while staying safe and healthy. With Insureyouknow.org, you can keep all of your travel documents and personal identification in one place for easy planning and smooth travels.
Coping After a Cancer Diagnosis: Finding Strength, Clarity, and Support
November 15, 2025
According to CDC data, nearly 39% of men and women will be diagnosed with cancer at some point during their lifetime. Finding out that you or a loved one has cancer can come as a shock and bring with it feelings of fear and anger. One challenge to treatment is that these emotions can make it difficult to process all of the information the doctor is presenting. Research shows that when emotions are high, a person’s decision-making ability is hindered, making it hard to choose a treatment plan.
Here are ways to help you cope after a cancer diagnosis, so that you can make the best decisions about your care.
Get the Facts
Gather as much information on your condition as you can. Not only will this help you make treatment decisions, but it can also feel empowering to become informed. Write down questions for your healthcare team as you think of them.
Questions to ask include:
- What kind of cancer do I have?
- Where is the cancer located?
- Has the cancer spread?
- Is this a curable form of cancer?
- What are my treatment options?
Bring a close family member or friend to your appointments for support and a second set of ears to help you remember what the doctors say.
Some people want all the facts while others want to let their healthcare providers make treatment decisions. Think about what works best for you before your appointments.
Be Honest About Your Well-Being
Now is the time to keep the lines of communication open between your doctors and loved ones. You may end up feeling alone if you sense that people are trying to protect you from your diagnosis, or if you try to be strong and hold in your feelings. Instead, be open and honest with everyone about your condition and what you’re feeling.
One in four individuals experiences depression and anxiety after a cancer diagnosis, so speaking up and seeking support early can make a meaningful difference.
“Education can be a powerful resource,” says Cynthia Brown, a breast cancer oncology nurse at Chester County Hospital in Pennsylvania. “Knowledge is power, and when you are more aware of the physical and mental symptoms you can experience throughout your cancer treatment, you can feel more confident in your ability to manage them, and be less afraid of the unknown.”
Accept Help When Offered
Let your loved ones help with errands, household tasks, meals, and taking you to appointments. It helps those you love to care for you and can be a way for them to cope during this difficult time.
To prevent those closest to you from burning out, accept help from anyone who asks if there’s anything they can do. Your loved ones will appreciate the extra help.
Some say that putting their lives in order helps them feel more in control of their well-being. Being involved in your treatment plan, keeping track of appointments, and making lifestyle changes are all things you can control.
While you can’t control every thought, you can choose which ones not to dwell on. Instead of worrying, for example, pay attention to the parts of life that bring you joy.
“As much as I’m in my own head thinking, ‘Cancer, cancer, cancer,’ and spiraling, my kids still have school pickup and drop-off, and they still want cuddle time,” says Stephanie Wysaski, a 35-year-old mother diagnosed with breast cancer. “I just didn’t have time to worry. Life doesn’t stop.”
Reevaluate Your Priorities
Receiving a cancer diagnosis can be a turning point in an individual’s life. Many people experience a new perspective and examine what they’ve been putting value on. Find more time for what matters most to you, and cancel everything that doesn’t align with your goals. Be open and honest with your loved ones about any changes you may be making and explain why.
Even when you don’t feel well, healthy lifestyle choices will constantly improve your energy level. Eating a nutritious diet, getting enough rest, and continuing to exercise as much as you can will help with the stress and fatigue that come with cancer and treatment. Setting a schedule and sticking to a routine helps manage daily exercise, getting enough sleep, and preparing healthy meals.
Expand Your Circle
It can be hard for people who don’t have cancer to understand precisely what you’re going through. That’s why talking to others in a similar situation can be so helpful. Cancer survivors can share their experiences and tell you what to expect during treatment.
You can try talking to someone you already know, like a friend or family member who has had cancer, or join a support group. To find a group, ask your healthcare provider or contact your local chapter of the American Cancer Society.
Care For Caregivers
The effect of a diagnosis can affect everyone in that person’s life, creating a ripple effect through families and communities. Seeking support through counseling or a caregiver support meeting can provide relief and guidance during a difficult time. Caregivers must take time for their own well-being and remember that it’s essential in caring for their loved one too.
“If someone in your life has been diagnosed with cancer, it’s okay to take time to process your feelings as well,” says Brown. “Those emotions are still important—even if the diagnosis isn’t yours. You may be worried for your loved one or angry about the disease. And if you are providing care for this person, you may experience feelings of stress or burnout.”
You may utilize Insureyouknow.org to organize your affairs, including finances, medical records, treatment, plans, and new schedules. Taking care of what you can control will eliminate unnecessary stress during treatment and recovery.
How to Choose a Medical Power of Attorney and Stay Prepared
November 6, 2025
A few years ago, a close friend of mine went through something that completely changed how I look at “being prepared.” Her dad had a stroke while working in the garden. One minute he was watering plants, the next, he was in the hospital, unable to speak. The doctors were asking who could make medical decisions for him, but no one had an answer. Everyone froze.
It was heartbreaking to watch. Her mom was in shock, her siblings were arguing, and everyone was scared. Nobody knew what he would have wanted.
That day taught me something that I’ll never forget. Planning ahead isn’t just about being responsible. It’s an act of love. And that’s exactly what a Medical Power of Attorney is all about.
What a Medical Power of Attorney Really Means
A Medical Power of Attorney (MPOA) sounds like a complicated legal thing, but it’s actually simple. It’s a document that lets you choose someone you trust to make healthcare decisions if you can’t.
That person, your agent, doesn’t suddenly take over your life. They only step in if you can’t speak for yourself. Their role is to protect your wishes and make sure what you want actually happens.
It’s one of those things we tend to put off, but once it’s done, it brings a quiet kind of comfort. You know things will be okay, even if you can’t explain what you want in the moment.
Why It Matters
If you don’t have a Medical Power of Attorney, hospitals usually turn to whoever’s nearby or follow state laws about next of kin. That can work, but it can also cause a lot of tension. In stressful moments, people don’t always think clearly. They guess, they argue, they panic.
Having an MPOA avoids all that. It gives doctors one clear person to speak with and gives your family direction when things feel uncertain. It’s a simple form, but it can prevent a lot of heartache later.
How to Choose the Right Person
Choosing your agent isn’t about who’s closest to you. It’s about who knows you best. The person you trust most doesn’t have to be family. It could be a friend, a sibling, or someone who simply understands you.
Here’s what to think about:
- Who stays calm under pressure?
- Who knows how you feel about medical care and quality of life?
- Who will listen to doctors carefully and ask good questions?
- Who will do what you want, even if others disagree?
Once you decide, talk to them. It doesn’t need to be formal or serious. Maybe just bring it up during a car ride or while cooking dinner. Tell them how you feel about certain treatments or what kind of care you’d want. These honest conversations matter so much more than any form.
Keeping Your Documents in Order
Once your form is signed, keep it somewhere easy to find. In an emergency, no one wants to dig through stacks of paper.
Here’s what to keep together:
- Your MPOA form (signed and dated).
- A Living Will or Advance Directive describing your medical preferences.
- A HIPAA release form so your agent can speak with doctors.
- Health insurance cards and policy info.
- Emergency contacts for family and doctors.
- Photo IDs for you and your agent.
I like to keep mine in a labeled folder at home and another copy saved online. It’s one of those “just in case” things that saves everyone stress later.
Why Digital Storage Helps
Paper gets lost. It gets packed in a box or tossed by accident. That’s why having a digital copy is smart.
A secure site like InsureYouKnow.org makes it easy to upload and store important documents safely. You can label them, share access with your agent, and know that if you ever need them, they’re right there. It’s simple, private, and safe.
It’s not about being tech savvy, it’s about being practical.
Keep It Updated
Life changes. People move, relationships shift, new doctors come into your life. Once a year, take five or ten minutes to check that your MPOA and other forms are still up to date.
It doesn’t take long, but it gives you peace of mind that everything’s current.
A Final Thought
Setting up a Medical Power of Attorney isn’t about expecting bad things to happen. It’s about kindness, for yourself and the people who love you.
Once it’s done, you can stop worrying. You’ll know that, no matter what happens, your family won’t be left guessing. They’ll already know because you cared enough to prepare.
It’s not just a document. It’s peace of mind, and maybe one of the most loving things you can do.
Love in the Final Chapter: Caring for a Loved One in Home Hospice
October 15, 2025

When it comes to end-of-life care, 71% of Americans believe the goal should be to help people die without pain, discomfort, and stress. The focus of hospice care is on quality of life and symptom management, and it is designed to provide comfort to individuals with a life expectancy of six months or less.
A team of medical professionals addresses the patient’s physical, psychological, and spiritual needs on a case-by-case basis, ensuring that every patient receives a care plan tailored to their specific needs. Care is most often delivered in the patient’s home, and the hospice team can support caregivers during this process.
Quality is Key
Hospice is end-of-life care, but that doesn’t mean someone receiving care will pass right away. While doctors recommend hospice when a patient only has six months or less to live and is no longer responding to curative treatments, many patients live longer. In such cases, what matters still is a patient’s quality of life, not quantity.
“Each person’s journey at the end of life is different,” says Jessica Kelly, a licensed hospice nurse in New York. “We tailor our care to meet those unique needs, whether that’s managing pain, supporting emotional well-being, or helping families share meaningful moments together.”
Home Care Takes a Toll
While it is nearly everyone’s preference to pass away in the comfort of their own home, the task of caregiving can be more than loved ones expect. “I do think that when patients are at home, they are in a peaceful environment,” says Parul Goyal, a palliative care physician. “It is comfortable for them. But it may not be comfortable for family members watching them take their last breath.”
The burden put on loved ones, especially spouses, can cause caregiver syndrome, which is characterized by the stress and burnout that comes from providing constant care to someone who is chronically or terminally ill.
“Our long-term-care system in this country is really using families, unpaid family members,” says Katherine Ornstein, a professor of geriatrics and palliative medicine at Mount Sinai. “What we really need to do is to broaden the support that individuals and families can have as they’re caring for individuals throughout the course of serious illness.”
Self-Care for Caregivers
Providing care to a hospice patient can be both rewarding and difficult. Social psychology researchers Richard Schulz and Joan Monin found that caregivers suffer when they witness their loved one’s suffering without feeling like they can remedy it. It becomes important not just to care for the patient but for caregivers to care for themselves as well.
One way to start accepting a terminal diagnosis is to begin getting a loved one’s affairs in order. It can be helpful to collect necessary documents and passwords and to begin sorting through possessions. Staying busy during the care process can help manage emotions as they arise.
Handling Grief
It’s easy to get paperwork and belongings in order. It’s not as easy to manage your grief. The loss of a loved one is among life‘s most significant stressors. Grief can affect every aspect of your health. While everyone’s experience is different, it is common to feel intense emotions during a loved one’s illness and after losing them.
Here are ways caregivers can take care after loss:
- Express your emotions. Bottling them up will only intensify them.
- Don’t put yourself on a timeline. People move forward at their own pace. Trust that your pain will lessen over time.
- Take care of yourself as you grieve. Eat nourishing meals, stay hydrated, and sleep enough.
- When you’re ready, exercise. It can reduce stress, tension, and sadness.
- Hospice providers make grief support groups available to anyone who has lost a loved one in hospice care.
- The Hospice Foundation also offers a newsletter to help during bereavement.
When to Seek Help
Most people find a way to adjust to their loss, but it is a painful and uncomfortable process. About 10% to 15% of people who are grieving have a complicated reaction to their loss. Grief experts agree that if grief is unmanageable, meaning someone has not returned to their pre-loss level of functioning within six to 12 months, it may be time to seek the professional help of a grief counselor. Your hospice team can help you find the care you need.
Handling a loved one’s affairs is one way caregivers can manage their grief. With Insureyouknow.org, you may organize financial documents, property records, and other documentation of personal effects. Getting everything in order can bring you some peace of mind during emotionally challenging times.
A Simple Guide to Choosing a Medical Power of Attorney
September 15, 2025

Studies show that the treatment wishes of patients vary greatly from those of their family members, yet only a third of Americans have a medical power of attorney in place. With a medical power of attorney, you can legally designate an agent to handle your medical decisions should you become unable to speak for yourself. It also includes instructions on the kinds of medical treatment you wish to receive.
Even if you do not know your wishes, a medical POA ensures that the person you trust can make those decisions for you. “A medical power of attorney is a pretty powerful document,” says William Raftis, attorney for Student Legal Services at Texas Tech. “It grants a person to make medical decisions on behalf of another person in the case that they are unable to make such a decision for themselves.”
Without a Document
When you don’t have a medical power of attorney and you are unable to tell the doctor your preferences, the following people would be legally authorized to make your healthcare decisions:
- A court-appointed guardian or conservator
- Your spouse or domestic partner
- One of your adult children or siblings
- A close friend
- Your nearest living relative
It’s important to know that if you have a medical POA and get married, then that document is revoked. If you do not want your spouse to act as your agent, then you must have a new medical power of attorney written up.
Choosing an Agent
To designate someone as your agent, you must sign a legal medical power of attorney document that names an agent and the healthcare decisions you’d like them to make if you become unable to. Your agent can decide whether or not to admit or discharge you from a hospital or nursing home, which treatments you receive, and who has access to your medical records.
Many people mistakenly believe that designating an agent and signing a medical POA grants that person the authority to make all of your healthcare decisions. But a medical power of attorney is only necessary if you become unable to make your own decisions.
Every state has its own legal requirements for medical POAs, such as witnesses and notarization, but you may not even need a lawyer to draw up a medical POA. Many states provide free forms through government websites. If your state does not offer forms online, consider inquiring with healthcare providers and hospitals, as they may also have forms available.
Comfort is Key
The person you designate to be your agent should be somebody whom you trust. They should be over 18 years of age and should not be a doctor or healthcare professional. The person you choose should be someone who you know will carry out your wishes. You should discuss your wishes with them in advance and ensure that they will be comfortable making those decisions on your behalf.
If it makes you more comfortable, you may appoint two people to serve as co-agents or a successive agent in case the first agent becomes unable to do so. Keep in mind that it may create confusion when multiple agents are involved in the decision-making process. Healthcare professionals may only be able to reach one agent in the event of an emergency, or agents may disagree about how to carry out your wishes best.
Make Those Decisions Now
In addition to choosing your agent, your medical power of attorney should state your wishes.
The medical POA should state:
- Whether or not you want to use machines to be kept alive or receive feeding tubes
- Name a legal guardian, if needed
- Whether or not you want to donate any organs in the event of your passing, and what to do with your remains
If at some point, you change your mind about any of your directives or who you’d like to be your agent, then you should have a new medical power of attorney drawn up.
Medical POA Safekeeping
You should always inform your agent of any changes made to a medical POA and make sure they have the most up-to-date copy. Then store your document in a safe but easily accessible location. A medical power of attorney should be stored in both a physical safe place at home and a secure digital platform. Provide your attorney with a copy, as well as your healthcare providers and other trusted loved ones.
Why Documentation Matters
Emergencies come without warning. Without documentation in place, confusion over what’s best for you will add stress to an already difficult circumstance. Every adult should have a medical power of attorney in place, even adult children going off to college. “Students are 18 and they are now legally adults,” says Raftis. “It’s really just a way to help empower the students to make sound medical decisions.”
Acting early guarantees that you will have the necessary support during an emergency. This proactive approach enables families to focus on their loved one’s care rather than paperwork. “It’s a gift to your family to get these plans in place,” says Sally Hurme, an elder law attorney in Virginia. “Why create chaos, indecision, confusion, frustration, turmoil =—all of these may happen if you don’t have advance directives.”
Being clear about how you want to be cared for doesn’t just protect you; it also ensures that you receive the care you need. It prevents your loved ones from having to make painful decisions on your behalf under emotional circumstances. In this way, a medical power of attorney provides peace of mind for both the individual and their loved ones. With Insureyouknow.org, you can store all of your medical records and healthcare documentation in one simple-to-review place, giving you more time to focus on what matters.
