Category: Caregiving
Intergenerational Care Benefits Everyone Involved
September 29, 2024

September is Intergeneration Month, launched by The Intergenerational Foundation, to connect generations and urge people from varying age groups to socialize. The idea behind recognizing Intergeneration Month each September is to promote learning from each other, such as gaining a better understanding of history and the challenges that separate generations. By connecting with different age groups across generations, unlikely friendships form between those who would otherwise never have communicated with each other.
People balancing raising young children and caring for aging parents may consider looking into what intergenerational daycare can offer. Facilities that provide both child care and senior care are on the rise, and that’s probably because, in addition to being a convenient solution for caretakers, the benefits to each age group are numerous.
If you’re considering Intergenerational Care for your loved ones, here’s everything you need to know.
What is Intergenerational Care?
Intergenerational care centers provide care for both young children and older adults. “It’s also referred to as a ‘shared site,’” says Merle Griff, the director of McKinley Center Intergenerational Project. “In many cases, there’s a senior area on one side of the building, a child care area on the other, and a hallway connecting the two. At various points during the day, they come together,” she says. The care provided can take on several forms, but at the core, it’s a service offered to multiple generations to provide care in one place across age groups.
The benefits of multi-generational care include forming connections between people who have a lot to teach one another and who would have otherwise never been allowed to meet. “It brings younger and older people together to increase social connectedness, enhance well-being for the benefit of all ages, and strengthen the web of support that is so integral to families and communities,” says Sheri Steinig, the director of Generations United. “People of different ages come together to learn, play, grow, and interact in planned intergenerational activities as well as through informal encounters,” she says.
The Different Kinds of Intergenerational Care
While intergenerational care means care across generations, the services provided vary. “There are many settings for intergenerational care,” says Steinig. “There can be programs at community centers and schools or care in daycare centers, retirement communities, nursing homes or assisted living and affordable housing,” she says. You may even provide intergenerational care in the form of a multigenerational household where more than two generations live. One in four American households are already multigenerational.
Intergenerational care centers look more like daycare facilities with adult daycare services or nursing home locations. “Each center is run their own way,” says Griff. “There are typically planned, structured interactions during the day,” she says. Both age groups are usually not combined for the entire day. Daily intergenerational activities may look like a combined sport, arts and crafts activity, comparison presentations between then and now, or even cradling opportunities, where seniors are paired with infants to rock and soothe to sleep. To date, there are fewer care centers than intergenerational programs. While there are only 150 sites across the country, care centers are expected to grow in popularity. For instance, The Mount Intergenerational Learning Center, a Seattle preschool within a nursing home, reports having over 400 children on their waiting list.
Intergenerational care programs are structured pairings between children of various ages and older adults. Programs such as these are designed to foster relationships between youth and seniors. It could be a pen pal program between elementary school kids and seniors, college students visiting nursing homes, multi-age choirs, or veterans going to schools to talk to students about their experiences.
To find a program such as this or a care center in your area, Generations United offers a search tool.
The Benefits of Intergenerational Bonds
Many grandparents live thousands of miles away from their grandchildren while aging adults live several states away from their children. According to a study from the University of California San Francisco, 43% of older adults report experiencing loneliness, and those who feel lonely are at a 59% increased risk of declining health.
That’s when intergenerational care can help. Older adults experience a sense of purpose and renewal after spending time with and helping young people. It helps seniors feel like they are not just receiving care but offering care. “Despite the dementia diagnosis, the maternal and paternal instincts can still kick in, and the seniors feel a sense of purpose,” says Jenna Hauss, the president of ONEgeneration. “They can care for others. They don’t always need to be cared for,” she says.
It isn’t just older generations that benefit from the connection. Children who spend time around older adults have fewer biases around such things as walkers and wheelchairs and become more comfortable with these differences. Multigenerational care promotes sensitivity among both age groups. Parents notice that their children are more empathetic, while older adults experience less loneliness, reduced agitation, and improved overall health.
Intergenerational care addresses two important needs: early childcare and the increasing demand for senior services, but the benefits of this combined service reap rewards far beyond caretaking. Research is proving that both age groups experience different perks from intergenerational connections. If this sounds like it might be the right fit for you and your loved ones, Insureyouknow.org can help you search for care by storing all of your research, financial information, and medical records in one easy-to-review place.
Understanding What Hospice Care Means
July 1, 2024

When treatment for serious illnesses is causing more side effects than benefits, or when health problems become compounded, then a patient and their family members may begin to wonder about hospice. “We recognized as people consider hospice, it’s highly emotional times,” says medical director for Austin Palliative Care Dr. Kate Tindall. “It might include worries and fears.” But one of the things she hears most often from patients and their families is that they wish they had started sooner. Understanding who qualifies for hospice and what it entails is the first part of deciding what might be best for those with terminal conditions.
What is Hospice Care?
Hospice is meant to care for people who have an anticipated life expectancy of 6 months or less, when there is no cure for their ailment, and the focus of their care shifts to the management of their symptoms and their quality of life. With hospice, the patient’s comfort and dignity become the priority, so treatment of the condition ends and treatment of the symptoms, such as pain management, begins. There are no age restrictions placed around hospice care, meaning any child, adolescent, or adult who has been diagnosed with a terminal illness qualifies for hospice care.
An individual does not need to be bedridden or already in their final days of life in order to receive hospice care. Other common misconceptions about hospice care are that it is designed to cure any illness or prolong life. It is also not meant to hasten death or replace any existing care, such as those already provided by a physician.
Determining When it’s Time for Hospice
Establishing care is most beneficial for the patient and their caregivers when it is taken advantage of earlier rather than later. Hospice can be used for months as long as eligibility has been met. Once there is a significant decline in physical or cognitive function, the goal for treatment should become to help that individual live comfortably and forgo anymore physically debilitating treatments that have been unsuccessful in curing or halting the illness.
Both individuals and their loved ones who would benefit from initiating hospice care are often unaware of the services or are uncomfortable asking about them. “It’s a hard conversation to have,” says professor of medicine and palliative care at the Duke University School of Medicine David Casarett. “Many people really want to continue aggressive treatment up until the very end.” While many wait for their providers to suggest it, it should be understood that if eligibility for hospice has been met, an individual and their caregivers can initiate hospice care on their own.
Establishing Hospice Care
In order to qualify for hospice care, a physician must certify that the patient is medically eligible, which means that the individual’s life expectancy is 6 months or less. Typically, the referral to hospice starts with the attending physician’s knowledge of that person’s medical history, while eligibility is then confirmed by the hospice physician. A hospice care team consists of professionals who are trained to treat physical, psychological, and the spiritual needs of the individual, while also providing support to family members and caregivers. Care is person-centered, with the importance being placed on the coordination of care, setting clear treatment goals, and communicating with all involved parties.
Receiving Care at Home
Hospice care is generally provided in the person’s home, whether it’s a personal residence or a care facility, such as a nursing home. “When people are close to the end of their lives, going to the hospital does not make them feel better anymore,” explains professor of medicine at the University of California Dr. Carly Zapata. “Because there’s not necessarily something that we can do to address their underlying illness.” Staying at home allows the individual to be around their personal things and close to their loved ones and pets, which can provide them with comfort during the end of their life.
What Does Hospice Care Include?
Hospice includes periodic visits to the patient and their family or caregivers but is available 24-7 if needed. Medication for symptom relief is administered, any medical equipment needed is provided, and toileting and other supplies such as diapers, wipes, wheelchairs, hospital beds are provided. What may surprise some people is that hospice patients may even receive physical and occupational therapy, speech-language pathology services, and dietary counseling.
If needed, short-term inpatient care may be established for those who cannot achieve adequate pain and symptom relief in their home setting. Short-term respite care may also become available to help family caregivers who are experiencing or are at risk for caregiver burnout. Bereavement care, or grief and loss counseling, is also offered to loved ones who may experience anticipatory grief. Grief counseling is available to family members for up to 13 months after the person’s death.
Paying for Hospice
The first step in finding a hospice agency is to search for ones that serve your county. If there are several options available, then it’s recommended to talk to more than one and see which agency will best fit the patient’s needs. Adequate research should be conducted since not all hospice agencies provide physical and occupational therapy.
Hospice is a medicare benefit that all Medicare enrollees qualify for, but it may also be covered through private insurance and by Medicaid in almost every state. Military families may receive hospice through Tricare, while veterans with the Veterans Health Administration Standard Medical Benefits Package are also eligible for hospice. Hospice agencies will also accept individual self-pay, while there are also non-profit organizations that provide hospice services free of charge.
Discontinuing Hospice Care
Though it is uncommon, if a patient does improve or their condition stabilizes, they may no longer meet medical eligibility for hospice. If this happens, the patient is discharged from the program. Another situation that sometimes arises is when a person elects to try a curative therapy, such as a clinical study for a new medication or procedure. In order to do that, the patient must withdraw from hospice through what is called revocation. Both children and veterans are exempt from being disqualified from hospice care if they choose to also pursue curative treatments. Any person may always re-enroll in hospice care at any time as long as they meet the medical eligibility.
Opting for Palliative Care
Individuals with chronic conditions or life-threatening illnesses may opt for palliative care, which doesn’t require people to stop their treatments. Palliative care is a combination of treatment and comfort care and can be an important bridge to hospice care if patients become eligible. Because transitioning to hospice care can be an emotional choice, palliative care providers often help patients prepare for that. Many people avoid palliative care because they think it is equal to giving up and that death is imminent, but studies show that for many, palliative care allows them to live longer, happier lives. This is due to the benefits of symptom management and spiritual support.
While hospice care can be difficult to accept, it can provide people with the best quality of life possible in their final days, as well as provide their loved ones with valued support. With Insureyouknow.org, you may keep track of all medical and financial records in one easy-to-review place so that you may focus on caring for your loved one, your family, and yourself during this period of their care.
Life After a Stroke: What You Should Know
May 21, 2024
A stroke affects the brain’s arteries and occurs when a blood vessel that brings blood to the brain gets blocked or ruptures. The area of the brain that is supplied with blood by the blocked or ruptured blood vessel doesn’t get the oxygen and nutrients it needs, and without oxygen, nerve cells are unable to function. Since the brain controls one’s ability to move, feel, and think, a stroke can cause injury to the brain that could affect any or all of these functions.
Everyone should know the signs of a stroke and seek immediate medical attention if you think you or someone around you is having a stroke. If you or someone you love has recently had a stroke, then it’s important to understand what happens next.
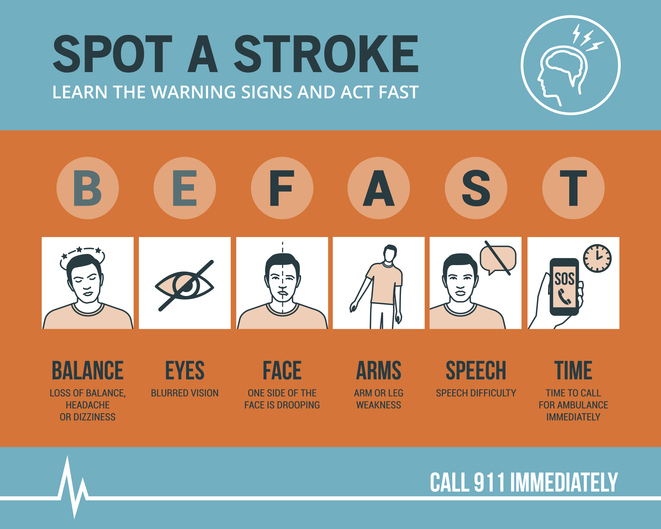
Know the Symptoms of a Stroke and act FAST
The longer the brain is left untreated during a stroke, the more likely it is that someone will have irreversible brain damage. The acronym FAST can help everyone recognize the four main signs that someone may be having a stroke and remember to act fast in seeking medical treatment. That means calling 9-1-1 immediately, as emergency response workers can treat someone on arrival if they think that person is having a stroke.
FAST stands for Facial drooping, Arm weakness, Speech difficulties, and most importantly, Time. If one side of a person’s face is drooping, if the person cannot lift both arms or one arm is drifting downward, and if the person’s speech is slurred or they cannot repeat a simple sentence, then they may be having a stroke. Not all of these signs need to be present to signal a stroke. Just one or two of these symptoms is enough to call 9-1-1, because time is of the essence in the event of a stroke.
Stroke Treatment Begins With Emergency Response Workers
Calling for an ambulance means that the emergency response workers can start life-saving treatment on the way to the hospital. Stroke patients who are taken to the hospital in an ambulance may get diagnosed and treated more quickly than people who wait to drive themselves. The emergency workers may also know best where to take someone, such as to a specialized stroke center to ensure that they receive the quickest possible treatment. The emergency workers can also collect valuable information for the hospital medical staff before the patient even gets to the emergency room, alerting staff of your arrival and allowing time to prepare. All of what the ambulance team can provide saves time in the treatment of stroke, and in the event of a stroke, time is of the essence.
Ischemic Stroke or Hemorrhagic Stroke?
There are two different kinds of stroke, ischemic or hemorrhagic. A medical team will need to determine which kind of stroke the patient is having in order to direct treatment. An ischemic stroke accounts for 87% of all strokes and happens when a blood clot blocks a vessel supplying blood to the brain. Hemorrhagic stroke happens when a blood vessel ruptures and bleeds within or around the brain.
“Fifty percent of strokes present with a clot in a large vessel in the brain, and these don’t respond very well to the old treatment, the IV clot busting medicine,” says M.D. and director of the Sparrow Comprehensive Stroke Center Anmar Razak. “And so nowadays, we do surgery, and what we do is we rush them into the hospital, into the cath lab. We quickly get access through the blood vessels and get up to where the clot is and pull it out.”
With ischemic stroke, the treatment goal is to dissolve or remove the clot. A medication called alteplase or tPA is often administered and works to dissolve the clot and enable blood flow. Alteplase saves lives and reduces the long-term effects of a stroke but must be given to the patient within three hours of the start of a stroke. Then, a procedure called mechanical thrombectomy removes the clot and must happen within six to 24 hours of stroke symptom onset.
For hemorrhagic stroke, the treatment goal is to stop the bleeding. There is a less-invasive endovascular procedure involving a catheter being threaded through a major artery in an arm or leg toward the area of the bleeding in the brain where a mechanism is inserted to prevent further rupture. In some cases, surgery is required to secure the blood vessel that has ruptured at the base of the bleeding.
Rehabilitation After a Stroke
Perhaps the most important part of stroke treatment is determining why it happened or the underlying causes of the stroke. Stroke risk factors include high blood pressure, which weakens arteries over time, smoking, diabetes, high cholesterol, physical inactivity, being overweight, heart disease including atrial fibrillation or aFib, excessive alcohol intake or illegal drug use, and sleep apnea. By making the right lifestyle choices and having a good medical management plan moving forward, the risk of another stroke can be greatly reduced.
That’s because if you have had a stroke, you are at high risk for having another one. One in four stroke survivors have another within five years, while the risk of stroke within 90 days of transient ischemic attack or TIA is as high as 17% with the greatest risk during the first week. This is why it becomes so important to determine the underlying causes of the initial stroke. Your doctor may give you medications to manage a condition, such as high blood pressure, and then recommend lifestyle changes, including a different diet and regular exercise.
Rehabilitation after a stroke begins in the hospital, often within only a day or 2 after the stroke. “There are so many things that patients need to fall into place to be functional and independent again after a stroke,” said Razak. “And they always come down to speed and time.” Rehabilitation can help with the transition from the hospital to home and can help prevent another stroke. Recovery time after a stroke is different for everyone and can take weeks, months, or even years. Some people may recover fully, while others may have long-term or lifelong disabilities. Stroke rehabilitation should be thought of as a balance between full recovery and learning how to live most effectively with some deficits that may not be recovered.
Difficulties from a stroke range from paralysis or weakness on one or both sides of the body, fatigue, trouble with cognitive functioning such as thinking and memory, seizures, and mental health issues like depression or anxiety from the fear of having another stroke. Everyone’s rehabilitation will look different based on their difficulties after a stroke but may include speech, physical, and occupational therapy. Speech therapy helps when someone is having problems producing or understanding speech, physical therapy uses exercises that help someone relearn movement and coordination skills, and occupational therapy focuses on improving daily activities, such as eating, dressing, and bathing. Joining a patient support group may help people adjust to life after a stroke, while support from family and friends can also help relieve the depression and anxiety following a stroke. It’s important for stroke patients to let their medical team and loved ones know how they’re feeling throughout their recovery and what they may need help with.
Stroke rehabilitation can be hard work, but just as in the initial treatment of a stroke, time matters in the possibility of a full recovery. Many survivors will tell you that rehabilitation is worth it and recommend using motivators to achieve recovery goals, such as wanting to see a child’s graduation or returning to working in the garden. With Insureyouknow.org, caretakers may keep track of medical treatments and rehabilitation plans in one easy-to-review place so that they may focus on caring for their loved one during the period of recovery from stroke.
May is American Stroke Month which aims to raise awareness of the second leading cause of death.
Looking after Elderly Parents Remotely
March 1, 2024

Taking care of loved ones without being close by is a challenge. Whether you live a long drive away from aging parents or in another state, long-distance caregiving can become emotionally exhausting. If that sounds like you, know that you are not alone. Nearly 15 percent of caregivers live an average of 450 miles away. If you have recently found yourself looking after your parents from a distance, then here are some simple strategies to help you along the way.
Evaluate Your Strengths and Outsource the Rest
Be honest with yourself about your strengths. Maybe you’re comfortable handling finances but not as comfortable determining medical needs. Pinpointing the areas of need that you’ll be most suitable for is the first step in delegating the rest. You may have siblings who live closer to your parents and are willing to accompany them to their doctor’s visits. Other helpful skills include organization and communication, which could be utilized to organize schedules and communicate with medical professionals and caregivers. Once you determine what you’ll be best at handling, then you can begin to make plans to fill in the gaps.
Create a Team for Support
Speak with the rest of your family and close friends about who can help with your parents’ care. Coordinating with everyone to determine what each person is willing to do will help everyone be on the same page and turn creating a care plan into a team effort. Even if you don’t have any other siblings or family members who are able to help, then you should still meet with your parents and include them in their own care planning. For instance, ask them what you can do that will be most helpful. It’s important to remember that you don’t have to handle everything alone and to try and outsource anything you need help with as much as possible.
Establish Access to Information
Once you determine who the primary caregivers will be and who needs to be in charge of what, then it’s time to make sure those people have access to the appropriate information. Make sure that the person designated to handle bill-paying and account management on behalf of your parents has the ability to do so. Establishing the rights to have medical information released to caregivers as well as decision-making rights is another imperative. This can also be a legal issue down the road, so making sure that you or another trusted party is the power of attorney, who is appointed to make financial and medical decisions, will need to be determined.
Revisit Living Arrangements
Sometimes a loved one’s health requires them to be closer to you. If it’s possible to relocate to where they live or have them move in with you, then that may be something worth exploring. If it’s not possible to live together, then senior living communities have the upside of being able to provide 24/7 care. Many older people don’t require full-time care though, so if relocation isn’t feasible, then hiring a home care aide or personal care assistant is another option.
Schedule Regular In-Person Visits
If you cannot live close to your parents, then making plans to see them will accomplish several things. First, you’ll instantly alleviate some of the caregiver guilt you may be experiencing just by knowing when you’ll be able to visit them next. Second, you’ll be able to check on them in-person, as you may not have an accurate assessment of their condition and needs from a distance. “It’s hard keeping a handle on their health, how they’re doing, physically, mentally, psychologically and emotionally, when you’re not there,” says Amy Goyer, AARP’s family and caregiving expert. “Isolation is a big thing and they can tell you, oh, I’m doing fine and everything on the phone, but is that really what’s happening?”
Lastly, but most importantly, you’ll be able to spend some much-needed quality time with your parents when visiting. If you are not the primary caregiver, then coordinate with them on when the best time to visit is and offer them a break. Plan in advance what you can do when you’re there to help out. Then speak with your parents about what they would like to do with you during your visit. Since visits can go by quickly, especially when there is so much to do, set priorities ahead of time about what’s most important once you’re there.
Remain Connected When You’re Apart
Schedule regular phone calls with your parents and ask for updates from their caregivers. With their permission, you may even choose to attend their telehealth visits and doctor’s appointments virtually. “The frequency of contact is dependent on the type and level of care needed,” says Iris Waichler, author of Role Reversal, How to Take Care of Yourself and Your Aging Parents. “It should be a collaborative decision, if possible, rather than a unilateral mandate from the caregiver.”
Regular communication can keep your bond with your parents strong, as long as it remains an enjoyable experience for all of you.
Take Care of Yourself as Well
Caregiving can come with a heavy emotional load. It will become just as important to check in with yourself in your new role as caregiver. “Caregivers may often feel like they can do more and this can cause ruminating thoughts,” says Brittany Ferri, geriatric care occupational therapist. “In this instance, they may benefit from practicing positive self-care and self-talk along with their loved one to keep the lines of communication open while relieving stress.”
It’s hard to be a good caregiver, when you’re running on empty, so taking care of yourself as well is just as important as taking care of those depending on you. Show yourself compassion, make sure you’re recharging, and be kind to yourself.
Insureyouknow.org
While it can be a challenge to care for your parents from a distance, that doesn’t mean it’s not manageable. By planning ahead and creating a care team, you can make sure your parents are cared for even when you can’t be close at all times. Insureyouknow.org can help you compile care plans, schedules, financial information, and medical records all in one place. Then you can rest easy that you have a plan set in motion, ensuring that your parents will be well-taken care of.
